Luuster, ik heb t denk ik. Het Corona-virus = n combinatie van het Influenza-virus,
Leukemie, alle soorten alle Kroon-virussen, Ebola-virus, AIDS/ HIV, Parkinson, Huntington, ALS, Heemi-plegia, Chlamydia, Bot-kanker, Maag-kanker. Dikke-darm-kanker, Colon-kanker, Dunne-darm-kanker, keel-kanker, Hemoraggische koorts, Dengue, & het Marburg-virus. Zo-iets, er wordt, aan mijn hoofd gezeurd, voor meer, maar ik vertrouw niemand, alleen me-zelf. Ik heb, alle voor-genoemde ziektes. Ik denk, dat er, daar-om iemand gedacht, heeft Raisie heeft het ook, dan kunnen andere unter-menschen, het ook aan.
_ ACEtwee gen verbergen
neus_druppels< zakdoeljes> anta flu
HIV/AIDS
| HIV/AIDS | |
|---|---|
| Other names | HIV disease, HIV infection[1][2] |
 | |
| The red ribbon is a symbol for solidarity with HIV-positive people and those living with AIDS.[3] | |
| Specialty | Infectious disease |
| Symptoms | Early: Flu-like illness[4] Later: Large lymph nodes, fever, weight loss[4] |
| Complications | Opportunistic infections, tumors[4] |
| Duration | Lifelong[4] |
| Causes | Human immunodeficiency virus (HIV)[4] |
| Risk factors | Exposure to blood, breast milk, sex[4] |
| Diagnostic method | Blood tests[4] |
| Prevention | Safe sex, needle exchange, male circumcision, pre-exposure prophylaxis, post-exposure prophylaxis[4] |
| Treatment | Antiretroviral therapy[4] |
| Prognosis | Near normal life expectancy with treatment[5][6] 11 years life expectancy without treatment[7] |
| Frequency | 1.7 million new cases (2018)[8] 37.9 million living with HIV (2018)[8] |
| Deaths | 770,000 (2018)[8] |
Human immunodeficiency virus infection and acquired immune deficiency syndrome (HIV/AIDS) is a spectrum of conditions caused by infection with the human immunodeficiency virus (HIV).[9][10][11] Following initial infection a person may not notice any symptoms, or may experience a brief period of influenza-like illness.[4] Typically, this is followed by a prolonged period with no symptoms.[5] If the infection progresses, it interferes more with the immune system, increasing the risk of developing common infections such as tuberculosis, as well as other opportunistic infections, and tumors which are otherwise rare in people who have normal immune function.[4] These late symptoms of infection are referred to as acquired immunodeficiency syndrome (AIDS).[5] This stage is often also associated with unintended weight loss.[5]
HIV is spread primarily by unprotected sex (including anal and oral sex), contaminated blood transfusions, hypodermic needles, and from mother to child during pregnancy, delivery, or breastfeeding.[12] Some bodily fluids, such as saliva, sweat and tears, do not transmit the virus.[13] HIV is a member of the group of viruses known as retroviruses.[14]
Methods of prevention include safe sex, needle exchange programs, treating those who are infected, pre- and post-exposure prophylaxis, and male circumcision.[4] Disease in a baby can often be prevented by giving both the mother and child antiretroviral medication.[4] There is no cure or vaccine; however, antiretroviral treatment can slow the course of the disease and may lead to a near-normal life expectancy.[5][6] Treatment is recommended as soon as the diagnosis is made.[15] Without treatment, the average survival time after infection is 11 years.[7]
In 2018 about 37.9 million people were living with HIV and it resulted in 770,000 deaths.[8] An estimated 20.6 million of these live in eastern and southern Africa.[16] Between the time that AIDS was identified (in the early 1980s) and 2018, the disease caused an estimated 32 million deaths worldwide.[8] HIV/AIDS is considered a pandemic—a disease outbreak which is present over a large area and is actively spreading.[17] HIV made the jump from other primates to humans in west-central Africa in the early-to-mid 20th century.[18] AIDS was first recognized by the United States Centers for Disease Control and Prevention (CDC) in 1981 and its cause—HIV infection—was identified in the early part of the decade.[19]
HIV/AIDS has had a large impact on society, both as an illness and as a source of discrimination.[20] The disease also has large economic impacts.[20] There are many misconceptions about HIV/AIDS, such as the belief that it can be transmitted by casual non-sexual contact.[21] The disease has become subject to many controversies involving religion, including the Catholic Church's position not to support condom use as prevention.[22] It has attracted international medical and political attention as well as large-scale funding since it was identified in the 1980s.[23]
Signs and symptoms
There are three main stages of HIV infection: acute infection, clinical latency, and AIDS.[1][24]
Acute infection
The initial period following the contraction of HIV is called acute HIV, primary HIV or acute retroviral syndrome.[24][25] Many individuals develop an influenza-like illness or a mononucleosis-like illness 2–4 weeks after exposure while others have no significant symptoms.[26][27] Symptoms occur in 40–90% of cases and most commonly include fever, large tender lymph nodes, throat inflammation, a rash, headache, tiredness, and/or sores of the mouth and genitals.[25][27] The rash, which occurs in 20–50% of cases, presents itself on the trunk and is maculopapular, classically.[28] Some people also develop opportunistic infections at this stage.[25] Gastrointestinal symptoms, such as vomiting or diarrhea may occur.[27] Neurological symptoms of peripheral neuropathy or Guillain–Barré syndrome also occurs.[27] The duration of the symptoms varies, but is usually one or two weeks.[27]
Owing to their nonspecific character, these symptoms are not often recognized as signs of HIV infection. Even cases that do get seen by a family doctor or a hospital are often misdiagnosed as one of the many common infectious diseases with overlapping symptoms. Thus, it is recommended that HIV be considered in people presenting with an unexplained fever who may have risk factors for the infection.[27]
Clinical latency
The initial symptoms are followed by a stage called clinical latency, asymptomatic HIV, or chronic HIV.[1] Without treatment, this second stage of the natural history of HIV infection can last from about three years[29] to over 20 years[30] (on average, about eight years).[31] While typically there are few or no symptoms at first, near the end of this stage many people experience fever, weight loss, gastrointestinal problems and muscle pains.[1] Between 50% and 70% of people also develop persistent generalized lymphadenopathy, characterized by unexplained, non-painful enlargement of more than one group of lymph nodes (other than in the groin) for over three to six months.[24]
Although most HIV-1 infected individuals have a detectable viral load and in the absence of treatment will eventually progress to AIDS, a small proportion (about 5%) retain high levels of CD4+ T cells (T helper cells) without antiretroviral therapy for more than five years.[27][32] These individuals are classified as "HIV controllers" or long-term nonprogressors (LTNP).[32] Another group consists of those who maintain a low or undetectable viral load without anti-retroviral treatment, known as "elite controllers" or "elite suppressors". They represent approximately 1 in 300 infected persons.[33]
Acquired immunodeficiency syndrome
Acquired immunodeficiency syndrome (AIDS) is defined as an HIV infection with either a CD4+ T cell count below 200 cells per µL or the occurrence of specific diseases associated with HIV infection.[27] In the absence of specific treatment, around half of people infected with HIV develop AIDS within ten years.[27] The most common initial conditions that alert to the presence of AIDS are pneumocystis pneumonia (40%), cachexia in the form of HIV wasting syndrome (20%), and esophageal candidiasis.[27] Other common signs include recurrent respiratory tract infections.[27]
Opportunistic infections may be caused by bacteria, viruses, fungi, and parasites that are normally controlled by the immune system.[34] Which infections occur depends partly on what organisms are common in the person's environment.[27] These infections may affect nearly every organ system.[35]
People with AIDS have an increased risk of developing various viral-induced cancers, including Kaposi's sarcoma, Burkitt's lymphoma, primary central nervous system lymphoma, and cervical cancer.[28] Kaposi's sarcoma is the most common cancer, occurring in 10% to 20% of people with HIV.[36] The second-most common cancer is lymphoma, which is the cause of death of nearly 16% of people with AIDS and is the initial sign of AIDS in 3% to 4%.[36] Both these cancers are associated with human herpesvirus 8 (HHV-8).[36] Cervical cancer occurs more frequently in those with AIDS because of its association with human papillomavirus (HPV).[36] Conjunctival cancer (of the layer that lines the inner part of eyelids and the white part of the eye) is also more common in those with HIV.[37]
Additionally, people with AIDS frequently have systemic symptoms such as prolonged fevers, sweats (particularly at night), swollen lymph nodes, chills, weakness, and unintended weight loss.[38] Diarrhea is another common symptom, present in about 90% of people with AIDS.[39] They can also be affected by diverse psychiatric and neurological symptoms independent of opportunistic infections and cancers.[40]
Transmission
| Exposure route | Chance of infection | |||
|---|---|---|---|---|
| Blood transfusion | 90%[41] | |||
| Childbirth (to child) | 25%[42][clarification needed] | |||
| Needle-sharing injection drug use | 0.67%[43] | |||
| Percutaneous needle stick | 0.30%[44] | |||
| Receptive anal intercourse* | 0.04–3.0%[45] | |||
| Insertive anal intercourse* | 0.03%[46] | |||
| Receptive penile-vaginal intercourse* | 0.05–0.30%[45][47] | |||
| Insertive penile-vaginal intercourse* | 0.01–0.38%[45][47] | |||
| Receptive oral intercourse*§ | 0–0.04%[45] | |||
| Insertive oral intercourse*§ | 0–0.005%[48] | |||
| * assuming no condom use § source refers to oral intercourse performed on a man | ||||
HIV is spread by three main routes: sexual contact, significant exposure to infected body fluids or tissues, and from mother to child during pregnancy, delivery, or breastfeeding (known as vertical transmission).[12] There is no risk of acquiring HIV if exposed to feces, nasal secretions, saliva, sputum, sweat, tears, urine, or vomit unless these are contaminated with blood.[49] It is also possible to be co-infected by more than one strain of HIV—a condition known as HIV superinfection.[50]
Sexual
The most frequent mode of transmission of HIV is through sexual contact with an infected person.[12] However, an HIV-positive person who has an undetectable viral load as a result of long-term treatment has effectively no risk of transmitting HIV sexually.[51][52] Globally, the most common mode of HIV transmission is via sexual contacts between people of the opposite sex;[12] however, the pattern of transmission varies among countries. As of 2017, most HIV transmission in the United States occurred among men who had sex with men (82% of new HIV diagnoses among males aged 13 and older and 70% of total new diagnoses).[53][54] In the US, gay and bisexual men aged 13 to 24 accounted for an estimated 92% of new HIV diagnoses among all men in their age group and 27% of new diagnoses among all gay and bisexual men.[55] About 15% of gay and bisexual men have HIV, while 28% of transgender women test positive in the US.[55][56]
With regard to unprotected heterosexual contacts, estimates of the risk of HIV transmission per sexual act appear to be four to ten times higher in low-income countries than in high-income countries.[57] In low-income countries, the risk of female-to-male transmission is estimated as 0.38% per act, and of male-to-female transmission as 0.30% per act; the equivalent estimates for high-income countries are 0.04% per act for female-to-male transmission, and 0.08% per act for male-to-female transmission.[57] The risk of transmission from anal intercourse is especially high, estimated as 1.4–1.7% per act in both heterosexual and homosexual contacts.[57][58] While the risk of transmission from oral sex is relatively low, it is still present.[59] The risk from receiving oral sex has been described as "nearly nil";[60] however, a few cases have been reported.[61] The per-act risk is estimated at 0–0.04% for receptive oral intercourse.[62] In settings involving prostitution in low-income countries, risk of female-to-male transmission has been estimated as 2.4% per act, and of male-to-female transmission as 0.05% per act.[57]
Risk of transmission increases in the presence of many sexually transmitted infections[63] and genital ulcers.[57] Genital ulcers appear to increase the risk approximately fivefold.[57] Other sexually transmitted infections, such as gonorrhea, chlamydia, trichomoniasis, and bacterial vaginosis, are associated with somewhat smaller increases in risk of transmission.[62]
The viral load of an infected person is an important risk factor in both sexual and mother-to-child transmission.[64] During the first 2.5 months of an HIV infection a person's infectiousness is twelve times higher due to the high viral load associated with acute HIV.[62] If the person is in the late stages of infection, rates of transmission are approximately eightfold greater.[57]
Commercial sex workers (including those in pornography) have an increased likelihood of contracting HIV.[65][66] Rough sex can be a factor associated with an increased risk of transmission.[67] Sexual assault is also believed to carry an increased risk of HIV transmission as condoms are rarely worn, physical trauma to the vagina or rectum is likely, and there may be a greater risk of concurrent sexually transmitted infections.[68]
Body fluids
The second-most frequent mode of HIV transmission is via blood and blood products.[12] Blood-borne transmission can be through needle-sharing during intravenous drug use, needle-stick injury, transfusion of contaminated blood or blood product, or medical injections with unsterilized equipment. The risk from sharing a needle during drug injection is between 0.63% and 2.4% per act, with an average of 0.8%.[69] The risk of acquiring HIV from a needle stick from an HIV-infected person is estimated as 0.3% (about 1 in 333) per act and the risk following mucous membrane exposure to infected blood as 0.09% (about 1 in 1000) per act.[49] This risk may, however, be up to 5% if the introduced blood was from a person with a high viral load and the cut was deep.[70] In the United States intravenous drug users made up 12% of all new cases of HIV in 2009,[71] and in some areas more than 80% of people who inject drugs are HIV-positive.[12]
HIV is transmitted in about 90% of blood transfusions using infected blood.[41] In developed countries the risk of acquiring HIV from a blood transfusion is extremely low (less than one in half a million) where improved donor selection and HIV screening is performed;[12] for example, in the UK the risk is reported at one in five million[72] and in the United States it was one in 1.5 million in 2008.[73] In low-income countries, only half of transfusions may be appropriately screened (as of 2008),[74] and it is estimated that up to 15% of HIV infections in these areas come from transfusion of infected blood and blood products, representing between 5% and 10% of global infections.[12][75] It is possible to acquire HIV from organ and tissue transplantation, although this is rare because of screening.[76]
Unsafe medical injections play a role in HIV spread in sub-Saharan Africa. In 2007, between 12% and 17% of infections in this region were attributed to medical syringe use.[77] The World Health Organization estimates the risk of transmission as a result of a medical injection in Africa at 1.2%.[77] Risks are also associated with invasive procedures, assisted delivery, and dental care in this area of the world.[77]
People giving or receiving tattoos, piercings, and scarification are theoretically at risk of infection but no confirmed cases have been documented.[78] It is not possible for mosquitoes or other insects to transmit HIV.[79]
Mother-to-child
HIV can be transmitted from mother to child during pregnancy, during delivery, or through breast milk, resulting in the baby also contracting HIV.[80][12] As of 2008, vertical transmission accounted for about 90% of cases of HIV in children.[81] In the absence of treatment, the risk of transmission before or during birth is around 20%, and in those who also breastfeed 35%.[81] Treatment decreases this risk to less than 5%.[82]
Antiretrovirals when taken by either the mother or the baby decrease the risk of transmission in those who do breastfeed.[83] If blood contaminates food during pre-chewing it may pose a risk of transmission.[78] If a woman is untreated, two years of breastfeeding results in an HIV/AIDS risk in her baby of about 17%.[84] Due to the increased risk of death without breastfeeding in many areas in the developing world, the World Health Organization recommends either exclusive breastfeeding or the provision of safe formula.[84] All women known to be HIV-positive should be taking lifelong antiretroviral therapy.[84]
Virology
HIV is the cause of the spectrum of disease known as HIV/AIDS. HIV is a retrovirus that primarily infects components of the human immune system such as CD4+ T cells, macrophages and dendritic cells. It directly and indirectly destroys CD4+ T cells.[85]
HIV is a member of the genus Lentivirus,[86] part of the family Retroviridae.[87] Lentiviruses share many morphological and biological characteristics. Many species of mammals are infected by lentiviruses, which are characteristically responsible for long-duration illnesses with a long incubation period.[88] Lentiviruses are transmitted as single-stranded, positive-sense, enveloped RNA viruses. Upon entry into the target cell, the viral RNA genome is converted (reverse transcribed) into double-stranded DNA by a virally encoded reverse transcriptase that is transported along with the viral genome in the virus particle. The resulting viral DNA is then imported into the cell nucleus and integrated into the cellular DNA by a virally encoded integrase and host co-factors.[89] Once integrated, the virus may become latent, allowing the virus and its host cell to avoid detection by the immune system.[90] Alternatively, the virus may be transcribed, producing new RNA genomes and viral proteins that are packaged and released from the cell as new virus particles that begin the replication cycle anew.[91]
HIV is now known to spread between CD4+ T cells by two parallel routes: cell-free spread and cell-to-cell spread, i.e. it employs hybrid spreading mechanisms.[92] In the cell-free spread, virus particles bud from an infected T cell, enter the blood/extracellular fluid and then infect another T cell following a chance encounter.[92] HIV can also disseminate by direct transmission from one cell to another by a process of cell-to-cell spread.[93][94] The hybrid spreading mechanisms of HIV contribute to the virus's ongoing replication against antiretroviral therapies.[92][95]
Two types of HIV have been characterized: HIV-1 and HIV-2. HIV-1 is the virus that was originally discovered (and initially referred to also as LAV or HTLV-III). It is more virulent, more infective,[96] and is the cause of the majority of HIV infections globally. The lower infectivity of HIV-2 as compared with HIV-1 implies that fewer people exposed to HIV-2 will be infected per exposure. Because of its relatively poor capacity for transmission, HIV-2 is largely confined to West Africa.[97]
Pathophysiology
After the virus enters the body there is a period of rapid viral replication, leading to an abundance of virus in the peripheral blood. During primary infection, the level of HIV may reach several million virus particles per milliliter of blood.[98] This response is accompanied by a marked drop in the number of circulating CD4+ T cells. The acute viremia is almost invariably associated with activation of CD8+ T cells, which kill HIV-infected cells, and subsequently with antibody production, or seroconversion. The CD8+ T cell response is thought to be important in controlling virus levels, which peak and then decline, as the CD4+ T cell counts recover. A good CD8+ T cell response has been linked to slower disease progression and a better prognosis, though it does not eliminate the virus.[99]
Ultimately, HIV causes AIDS by depleting CD4+ T cells. This weakens the immune system and allows opportunistic infections. T cells are essential to the immune response and without them, the body cannot fight infections or kill cancerous cells. The mechanism of CD4+ T cell depletion differs in the acute and chronic phases.[100] During the acute phase, HIV-induced cell lysis and killing of infected cells by CD8+ T cells accounts for CD4+ T cell depletion, although apoptosis may also be a factor. During the chronic phase, the consequences of generalized immune activation coupled with the gradual loss of the ability of the immune system to generate new T cells appear to account for the slow decline in CD4+ T cell numbers.[101]
Although the symptoms of immune deficiency characteristic of AIDS do not appear for years after a person is infected, the bulk of CD4+ T cell loss occurs during the first weeks of infection, especially in the intestinal mucosa, which harbors the majority of the lymphocytes found in the body.[102] The reason for the preferential loss of mucosal CD4+ T cells is that the majority of mucosal CD4+ T cells express the CCR5 protein which HIV uses as a co-receptor to gain access to the cells, whereas only a small fraction of CD4+ T cells in the bloodstream do so.[103] A specific genetic change that alters the CCR5 protein when present in both chromosomes very effectively prevents HIV-1 infection.[104]
HIV seeks out and destroys CCR5 expressing CD4+ T cells during acute infection.[105] A vigorous immune response eventually controls the infection and initiates the clinically latent phase. CD4+ T cells in mucosal tissues remain particularly affected.[105] Continuous HIV replication causes a state of generalized immune activation persisting throughout the chronic phase.[106] Immune activation, which is reflected by the increased activation state of immune cells and release of pro-inflammatory cytokines, results from the activity of several HIV gene products and the immune response to ongoing HIV replication. It is also linked to the breakdown of the immune surveillance system of the gastrointestinal mucosal barrier caused by the depletion of mucosal CD4+ T cells during the acute phase of disease.[107]
Diagnosis
| Blood test | Days |
|---|---|
| Antibody test (rapid test, ELISA 3rd gen) | 23–90 |
| Antibody and p24 antigen test (ELISA 4th gen) | 18–45 |
| PCR | 10–33 |
HIV/AIDS is diagnosed via laboratory testing and then staged based on the presence of certain signs or symptoms.[25] HIV screening is recommended by the United States Preventive Services Task Force for all people 15 years to 65 years of age, including all pregnant women.[109] Additionally, testing is recommended for those at high risk, which includes anyone diagnosed with a sexually transmitted illness.[28][109] In many areas of the world, a third of HIV carriers only discover they are infected at an advanced stage of the disease when AIDS or severe immunodeficiency has become apparent.[28]
HIV testing
Most people infected with HIV develop specific antibodies (i.e. seroconvert) within three to twelve weeks after the initial infection.[27] Diagnosis of primary HIV before seroconversion is done by measuring HIV-RNA or p24 antigen.[27] Positive results obtained by antibody or PCR testing are confirmed either by a different antibody or by PCR.[25]
Antibody tests in children younger than 18 months are typically inaccurate, due to the continued presence of maternal antibodies.[110] Thus HIV infection can only be diagnosed by PCR testing for HIV RNA or DNA, or via testing for the p24 antigen.[25] Much of the world lacks access to reliable PCR testing, and people in many places simply wait until either symptoms develop or the child is old enough for accurate antibody testing.[110] In sub-Saharan Africa between 2007 and 2009, between 30% and 70% of the population were aware of their HIV status.[111] In 2009, between 3.6% and 42% of men and women in sub-Saharan countries were tested;[111] this represented a significant increase compared to previous years.[111]
Classifications
Two main clinical staging systems are used to classify HIV and HIV-related disease for surveillance purposes: the WHO disease staging system for HIV infection and disease,[25] and the CDC classification system for HIV infection.[112] The CDC's classification system is more frequently adopted in developed countries. Since the WHO's staging system does not require laboratory tests, it is suited to the resource-restricted conditions encountered in developing countries, where it can also be used to help guide clinical management. Despite their differences, the two systems allow comparison for statistical purposes.[24][25][112]
The World Health Organization first proposed a definition for AIDS in 1986.[25] Since then, the WHO classification has been updated and expanded several times, with the most recent version being published in 2007.[25] The WHO system uses the following categories:
- Primary HIV infection: May be either asymptomatic or associated with acute retroviral syndrome[25]
- Stage I: HIV infection is asymptomatic with a CD4+ T cell count (also known as CD4 count) greater than 500 per microlitre (µl or cubic mm) of blood.[25] May include generalized lymph node enlargement.[25]
- Stage II: Mild symptoms, which may include minor mucocutaneous manifestations and recurrent upper respiratory tract infections. A CD4 count of less than 500/µl[25]
- Stage III: Advanced symptoms, which may include unexplained chronic diarrhea for longer than a month, severe bacterial infections including tuberculosis of the lung, and a CD4 count of less than 350/µl[25]
- Stage IV or AIDS: severe symptoms, which include toxoplasmosis of the brain, candidiasis of the esophagus, trachea, bronchi, or lungs, and Kaposi's sarcoma. A CD4 count of less than 200/µl[25]
The United States Center for Disease Control and Prevention also created a classification system for HIV, and updated it in 2008 and 2014.[112][113] This system classifies HIV infections based on CD4 count and clinical symptoms, and describes the infection in five groups.[113] In those greater than six years of age it is:[113]
- Stage 0: the time between a negative or indeterminate HIV test followed less than 180 days by a positive test.
- Stage 1: CD4 count ≥ 500 cells/µl and no AIDS-defining conditions.
- Stage 2: CD4 count 200 to 500 cells/µl and no AIDS-defining conditions.
- Stage 3: CD4 count ≤ 200 cells/µl or AIDS-defining conditions.
- Unknown: if insufficient information is available to make any of the above classifications.
For surveillance purposes, the AIDS diagnosis still stands even if, after treatment, the CD4+ T cell count rises to above 200 per µL of blood or other AIDS-defining illnesses are cured.[24]
Prevention
Consistent condom use reduces the risk of HIV transmission by approximately 80% over the long term.[114] When condoms are used consistently by a couple in which one person is infected, the rate of HIV infection is less than 1% per year.[115] There is some evidence to suggest that female condoms may provide an equivalent level of protection.[116] Application of a vaginal gel containing tenofovir (a reverse transcriptase inhibitor) immediately before sex seems to reduce infection rates by approximately 40% among African women.[117] By contrast, use of the spermicide nonoxynol-9 may increase the risk of transmission due to its tendency to cause vaginal and rectal irritation.[118]
Circumcision in Sub-Saharan Africa "reduces the acquisition of HIV by heterosexual men by between 38% and 66% over 24 months".[119] Owing to these studies, both the World Health Organization and UNAIDS recommended male circumcision in 2007 as a method of preventing female-to-male HIV transmission in areas with high rates of HIV.[120] However, whether it protects against male-to-female transmission is disputed,[121][122] and whether it is of benefit in developed countries and among men who have sex with men is undetermined.[123][124][125] The International Antiviral Society, however, does recommend it for all sexually active heterosexual males and that it be discussed as an option with men who have sex with men.[126] Some experts fear that a lower perception of vulnerability among circumcised men may cause more sexual risk-taking behavior, thus negating its preventive effects.[127]
Programs encouraging sexual abstinence do not appear to affect subsequent HIV risk.[128] Evidence of any benefit from peer education is equally poor.[129] Comprehensive sexual education provided at school may decrease high-risk behavior.[130][131] A substantial minority of young people continues to engage in high-risk practices despite knowing about HIV/AIDS, underestimating their own risk of becoming infected with HIV.[132] Voluntary counseling and testing people for HIV does not affect risky behavior in those who test negative but does increase condom use in those who test positive.[133] Enhanced family planning services appear to increase the likelihood of women with HIV using contraception, compared to basic services.[134] It is not known whether treating other sexually transmitted infections is effective in preventing HIV.[63]
Pre-exposure
Antiretroviral treatment among people with HIV whose CD4 count ≤ 550 cells/µL is a very effective way to prevent HIV infection of their partner (a strategy known as treatment as prevention, or TASP).[135] TASP is associated with a 10- to 20-fold reduction in transmission risk.[135][136] Pre-exposure prophylaxis (PrEP) with a daily dose of the medications tenofovir, with or without emtricitabine, is effective in people at high risk including men who have sex with men, couples where one is HIV-positive, and young heterosexuals in Africa.[117][137] It may also be effective in intravenous drug users, with a study finding a decrease in risk of 0.7 to 0.4 per 100 person years.[138] The USPSTF, in 2019, recommended PrEP in those who are at high risk.[139]
Universal precautions within the health care environment are believed to be effective in decreasing the risk of HIV.[140] Intravenous drug use is an important risk factor, and harm reduction strategies such as needle-exchange programs and opioid substitution therapy appear effective in decreasing this risk.[141][142]
Post-exposure
A course of antiretrovirals administered within 48 to 72 hours after exposure to HIV-positive blood or genital secretions is referred to as post-exposure prophylaxis (PEP).[143] The use of the single agent zidovudine reduces the risk of a HIV infection five-fold following a needle-stick injury.[143] As of 2013, the prevention regimen recommended in the United States consists of three medications—tenofovir, emtricitabine and raltegravir—as this may reduce the risk further.[144]
PEP treatment is recommended after a sexual assault when the perpetrator is known to be HIV-positive, but is controversial when their HIV status is unknown.[145] The duration of treatment is usually four weeks[146] and is frequently associated with adverse effects—where zidovudine is used, about 70% of cases result in adverse effects such as nausea (24%), fatigue (22%), emotional distress (13%) and headaches (9%).[49]
Mother-to-child
Programs to prevent the vertical transmission of HIV (from mothers to children) can reduce rates of transmission by 92–99%.[81][141] This primarily involves the use of a combination of antiviral medications during pregnancy and after birth in the infant, and potentially includes bottle feeding rather than breastfeeding.[81][147] If replacement feeding is acceptable, feasible, affordable, sustainable and safe, mothers should avoid breastfeeding their infants; however, exclusive breastfeeding is recommended during the first months of life if this is not the case.[148] If exclusive breastfeeding is carried out, the provision of extended antiretroviral prophylaxis to the infant decreases the risk of transmission.[149] In 2015, Cuba became the first country in the world to eradicate mother-to-child transmission of HIV.[150]
Vaccination
Currently there is no licensed vaccine for HIV or AIDS.[6] The most effective vaccine trial to date, RV 144, was published in 2009; it found a partial reduction in the risk of transmission of roughly 30%, stimulating some hope in the research community of developing a truly effective vaccine.[151] Further trials of the RV 144 vaccine are ongoing.[152][153]
Treatment
There is currently no cure, nor an effective HIV vaccine. Treatment consists of highly active antiretroviral therapy (HAART) which slows progression of the disease.[154] As of 2010 more than 6.6 million people were receiving this in low- and middle-income countries.[155] Treatment also includes preventive and active treatment of opportunistic infections. As of March 2020, two persons have been successfully cleared of HIV.[156]
Antiviral therapy
Current HAART options are combinations (or "cocktails") consisting of at least three medications belonging to at least two types, or "classes", of antiretroviral agents.[157] Initially, treatment is typically a non-nucleoside reverse transcriptase inhibitor (NNRTI) plus two nucleoside analog reverse transcriptase inhibitors (NRTIs).[158] Typical NRTIs include: zidovudine (AZT) or tenofovir (TDF) and lamivudine (3TC) or emtricitabine (FTC).[158] As of 2019, dolutegravir/lamivudine/tenofovir is listed by the World Health Organization as the first-line treatment for adults, with tenofovir/lamivudine/efavirenz as an alternative.[159] Combinations of agents that include protease inhibitors (PI) are used if the above regimen loses effectiveness.[157]
The World Health Organization and the United States recommend antiretrovirals in people of all ages (including pregnant women) as soon as the diagnosis is made, regardless of CD4 count.[15][126][160] Once treatment is begun, it is recommended that it is continued without breaks or "holidays".[28] Many people are diagnosed only after treatment ideally should have begun.[28] The desired outcome of treatment is a long-term plasma HIV-RNA count below 50 copies/mL.[28] Levels to determine if treatment is effective are initially recommended after four weeks and once levels fall below 50 copies/mL checks every three to six months are typically adequate.[28] Inadequate control is deemed to be greater than 400 copies/mL.[28] Based on these criteria treatment is effective in more than 95% of people during the first year.[28]
Benefits of treatment include a decreased risk of progression to AIDS and a decreased risk of death.[161] In the developing world, treatment also improves physical and mental health.[162] With treatment, there is a 70% reduced risk of acquiring tuberculosis.[157] Additional benefits include a decreased risk of transmission of the disease to sexual partners and a decrease in mother-to-child transmission.[157][163] The effectiveness of treatment depends to a large part on compliance.[28] Reasons for non-adherence to treatment include poor access to medical care,[164] inadequate social supports, mental illness and drug abuse.[165] The complexity of treatment regimens (due to pill numbers and dosing frequency) and adverse effects may reduce adherence.[166] Even though cost is an important issue with some medications,[167] 47% of those who needed them were taking them in low- and middle-income countries as of 2010,[155] and the rate of adherence is similar in low-income and high-income countries.[168]
Specific adverse events are related to the antiretroviral agent taken.[169] Some relatively common adverse events include: lipodystrophy syndrome, dyslipidemia, and diabetes mellitus, especially with protease inhibitors.[24] Other common symptoms include diarrhea,[169][170] and an increased risk of cardiovascular disease.[171] Newer recommended treatments are associated with fewer adverse effects.[28] Certain medications may be associated with birth defects and therefore may be unsuitable for women hoping to have children.[28]
Treatment recommendations for children are somewhat different from those for adults. The World Health Organization recommends treating all children less than 5 years of age; children above 5 are treated like adults.[172] The United States guidelines recommend treating all children less than 12 months of age and all those with HIV RNA counts greater than 100,000 copies/mL between one year and five years of age.[173]
Opportunistic infections
Measures to prevent opportunistic infections are effective in many people with HIV/AIDS. In addition to improving current disease, treatment with antiretrovirals reduces the risk of developing additional opportunistic infections.[169] Adults and adolescents who are living with HIV (even on anti-retroviral therapy) with no evidence of active tuberculosis in settings with high tuberculosis burden should receive isoniazid preventive therapy (IPT); the tuberculin skin test can be used to help decide if IPT is needed.[174] Vaccination against hepatitis A and B is advised for all people at risk of HIV before they become infected; however, it may also be given after infection.[175] Trimethoprim/sulfamethoxazole prophylaxis between four and six weeks of age, and ceasing breastfeeding of infants born to HIV-positive mothers, is recommended in resource-limited settings.[176] It is also recommended to prevent PCP when a person's CD4 count is below 200 cells/uL and in those who have or have previously had PCP.[177] People with substantial immunosuppression are also advised to receive prophylactic therapy for toxoplasmosis and MAC.[178] Appropriate preventive measures reduced the rate of these infections by 50% between 1992 and 1997.[179] Influenza vaccination and pneumococcal polysaccharide vaccine are often recommended in people with HIV/AIDS with some evidence of benefit.[180][181]
Diet
The World Health Organization (WHO) has issued recommendations regarding nutrient requirements in HIV/AIDS.[182] A generally healthy diet is promoted. Dietary intake of micronutrients at RDA levels by HIV-infected adults is recommended by the WHO; higher intake of vitamin A, zinc, and iron can produce adverse effects in HIV-positive adults, and is not recommended unless there is documented deficiency.[182][183][184][185] Dietary supplementation for people who are infected with HIV and who have inadequate nutrition or dietary deficiencies may strengthen their immune systems or help them recover from infections; however, evidence indicating an overall benefit in morbidity or reduction in mortality is not consistent.[186]
Evidence for supplementation with selenium is mixed with some tentative evidence of benefit.[187] For pregnant and lactating women with HIV, multivitamin supplement improves outcomes for both mothers and children.[188] If the pregnant or lactating mother has been advised to take anti-retroviral medication to prevent mother-to-child HIV transmission, multivitamin supplements should not replace these treatments.[188] There is some evidence that vitamin A supplementation in children with an HIV infection reduces mortality and improves growth.[189]
Alternative medicine
In the US, approximately 60% of people with HIV use various forms of complementary or alternative medicine,[190] whose effectiveness has not been established.[191] There is not enough evidence to support the use of herbal medicines.[192] There is insufficient evidence to recommend or support the use of medical cannabis to try to increase appetite or weight gain.[193]
Prognosis
HIV/AIDS has become a chronic rather than an acutely fatal disease in many areas of the world.[194] Prognosis varies between people, and both the CD4 count and viral load are useful for predicted outcomes.[27] Without treatment, average survival time after infection with HIV is estimated to be 9 to 11 years, depending on the HIV subtype.[7] After the diagnosis of AIDS, if treatment is not available, survival ranges between 6 and 19 months.[195][196] HAART and appropriate prevention of opportunistic infections reduces the death rate by 80%, and raises the life expectancy for a newly diagnosed young adult to 20–50 years.[194][197][198] This is between two thirds[197] and nearly that of the general population.[28][199] If treatment is started late in the infection, prognosis is not as good:[28] for example, if treatment is begun following the diagnosis of AIDS, life expectancy is ~10–40 years.[28][194] Half of infants born with HIV die before two years of age without treatment.[176]
The primary causes of death from HIV/AIDS are opportunistic infections and cancer, both of which are frequently the result of the progressive failure of the immune system.[179][200] Risk of cancer appears to increase once the CD4 count is below 500/μL.[28] The rate of clinical disease progression varies widely between individuals and has been shown to be affected by a number of factors such as a person's susceptibility and immune function;[201] their access to health care, the presence of co-infections;[195][202] and the particular strain (or strains) of the virus involved.[203][204]
Tuberculosis co-infection is one of the leading causes of sickness and death in those with HIV/AIDS being present in a third of all HIV-infected people and causing 25% of HIV-related deaths.[205] HIV is also one of the most important risk factors for tuberculosis.[206] Hepatitis C is another very common co-infection where each disease increases the progression of the other.[207] The two most common cancers associated with HIV/AIDS are Kaposi's sarcoma and AIDS-related non-Hodgkin's lymphoma.[200] Other cancers that are more frequent include anal cancer, Burkitt's lymphoma, primary central nervous system lymphoma, and cervical cancer.[28][208]
Even with anti-retroviral treatment, over the long term HIV-infected people may experience neurocognitive disorders,[209] osteoporosis,[210] neuropathy,[211] cancers,[212][213] nephropathy,[214] and cardiovascular disease.[170] Some conditions, such as lipodystrophy, may be caused both by HIV and its treatment.[170]
Epidemiology
HIV/AIDS is a global pandemic.[216] As of 2016 approximately 36.7 million people worldwide have HIV, the number of new infections that year being about 1.8 million.[217] This is down from 3.1 million new infections in 2001.[218] Slightly over half the infected population are women and 2.1 million are children.[217] It resulted in about 1 million deaths in 2016, down from a peak of 1.9 million in 2005.[217]
Sub-Saharan Africa is the region most affected. In 2010, an estimated 68% (22.9 million) of all HIV cases and 66% of all deaths (1.2 million) occurred in this region.[219] This means that about 5% of the adult population is infected[220] and it is believed to be the cause of 10% of all deaths in children.[221] Here, in contrast to other regions, women comprise nearly 60% of cases.[219] South Africa has the largest population of people with HIV of any country in the world at 5.9 million.[219] Life expectancy has fallen in the worst-affected countries due to HIV/AIDS; for example, in 2006 it was estimated that it had dropped from 65 to 35 years in Botswana.[17] Mother-to-child transmission in Botswana and South Africa, as of 2013, has decreased to less than 5%, with improvement in many other African nations due to improved access to antiretroviral therapy.[222]
South & South East Asia is the second most affected; in 2010 this region contained an estimated 4 million cases or 12% of all people living with HIV resulting in approximately 250,000 deaths.[220] Approximately 2.4 million of these cases are in India.[219]
During 2008 in the United States approximately 1.2 million people were living with HIV, resulting in about 17,500 deaths. The US Centers for Disease Control and Prevention estimated that in that year, 20% of infected Americans were unaware of their infection.[223] As of 2016 about 675,000 people have died of HIV/AIDS in the US since the beginning of the HIV epidemic.[56] In the United Kingdom as of 2015, there were approximately 101,200 cases which resulted in 594 deaths.[224] In Canada as of 2008, there were about 65,000 cases causing 53 deaths.[225] Between the first recognition of AIDS (in 1981) and 2009, it has led to nearly 30 million deaths.[226] Rates of HIV are lowest in North Africa and the Middle East (0.1% or less), East Asia (0.1%), and Western and Central Europe (0.2%).[220] The worst-affected European countries, in 2009 and 2012 estimates, are Russia, Ukraine, Latvia, Moldova, Portugal and Belarus, in decreasing order of prevalence.[227]
History
Discovery
AIDS was first clinically reported on June 5, 1981, with five cases in the United States.[36][228] The initial cases were a cluster of injecting drug users and homosexual men with no known cause of impaired immunity who showed symptoms of Pneumocystis carinii pneumonia (PCP), a rare opportunistic infection that was known to occur in people with very compromised immune systems.[229] Soon thereafter, an unexpected number of homosexual men developed a previously rare skin cancer called Kaposi's sarcoma (KS).[230][231] Many more cases of PCP and KS emerged, alerting U.S. Centers for Disease Control and Prevention (CDC) and a CDC task force was formed to monitor the outbreak.[232]
In the early days, the CDC did not have an official name for the disease, often referring to it by way of the diseases that were associated with it, for example, lymphadenopathy, the disease after which the discoverers of HIV originally named the virus.[233][234] They also used Kaposi's sarcoma and opportunistic infections, the name by which a task force had been set up in 1981.[235] At one point the CDC coined the phrase "the 4H disease", for the syndrome seemed to affect heroin users, homosexuals, hemophiliacs, and Haitians.[236][237] In the general press the term GRID, which stood for gay-related immune deficiency, had been coined.[238] However, after determining that AIDS was not isolated to the gay community,[235] it was realized that the term GRID was misleading, and the term AIDS was introduced at a meeting in July 1982.[239] By September 1982 the CDC started referring to the disease as AIDS.[240]
In 1983, two separate research groups led by Robert Gallo and Luc Montagnier declared that a novel retrovirus may have been infecting people with AIDS, and published their findings in the same issue of the journal Science.[241][242] Gallo claimed a virus which his group had isolated from a person with AIDS was strikingly similar in shape to other human T-lymphotropic viruses (HTLVs) that his group had been the first to isolate. Gallo's group called their newly isolated virus HTLV-III. At the same time, Montagnier's group isolated a virus from a person presenting with swelling of the lymph nodes of the neck and physical weakness, two characteristic symptoms of AIDS. Contradicting the report from Gallo's group, Montagnier and his colleagues showed that core proteins of this virus were immunologically different from those of HTLV-I. Montagnier's group named their isolated virus lymphadenopathy-associated virus (LAV).[232] As these two viruses turned out to be the same, in 1986, LAV and HTLV-III were renamed HIV.[243]
Origins
Both HIV-1 and HIV-2 are believed to have originated in non-human primates in West-central Africa and were transferred to humans in the early 20th century.[18] HIV-1 appears to have originated in southern Cameroon through the evolution of SIV(cpz), a simian immunodeficiency virus (SIV) that infects wild chimpanzees (HIV-1 descends from the SIVcpz endemic in the chimpanzee subspecies Pan troglodytes troglodytes).[244][245] The closest relative of HIV-2 is SIV(smm), a virus of the sooty mangabey (Cercocebus atys atys), an Old World monkey living in coastal West Africa (from southern Senegal to western Ivory Coast).[97] New World monkeys such as the owl monkey are resistant to HIV-1 infection, possibly because of a genomic fusion of two viral resistance genes.[246] HIV-1 is thought to have jumped the species barrier on at least three separate occasions, giving rise to the three groups of the virus, M, N, and O.[247]
There is evidence that humans who participate in bushmeat activities, either as hunters or as bushmeat vendors, commonly acquire SIV.[248] However, SIV is a weak virus which is typically suppressed by the human immune system within weeks of infection. It is thought that several transmissions of the virus from individual to individual in quick succession are necessary to allow it enough time to mutate into HIV.[249] Furthermore, due to its relatively low person-to-person transmission rate, SIV can only spread throughout the population in the presence of one or more high-risk transmission channels, which are thought to have been absent in Africa before the 20th century.
Specific proposed high-risk transmission channels, allowing the virus to adapt to humans and spread throughout the society, depend on the proposed timing of the animal-to-human crossing. Genetic studies of the virus suggest that the most recent common ancestor of the HIV-1 M group dates back to c. 1910.[250] Proponents of this dating link the HIV epidemic with the emergence of colonialism and growth of large colonial African cities, leading to social changes, including a higher degree of sexual promiscuity, the spread of prostitution, and the accompanying high frequency of genital ulcer diseases (such as syphilis) in nascent colonial cities.[251] While transmission rates of HIV during vaginal intercourse are low under regular circumstances, they are increased manyfold if one of the partners suffers from a sexually transmitted infection causing genital ulcers. Early 1900s colonial cities were notable for their high prevalence of prostitution and genital ulcers, to the degree that, as of 1928, as many as 45% of female residents of eastern Kinshasa were thought to have been prostitutes, and, as of 1933, around 15% of all residents of the same city had syphilis.[251]
An alternative view holds that unsafe medical practices in Africa after World War II, such as unsterile reuse of single-use syringes during mass vaccination, antibiotic and anti-malaria treatment campaigns, were the initial vector that allowed the virus to adapt to humans and spread.[249][252][253]
The earliest well-documented case of HIV in a human dates back to 1959 in the Congo.[254] The earliest retrospectively described case of AIDS is believed to have been in Norway beginning in 1966.[255] In July 1960, in the wake of Congo's independence, the United Nations recruited Francophone experts and technicians from all over the world to assist in filling administrative gaps left by Belgium, who did not leave behind an African elite to run the country. By 1962, Haitians made up the second-largest group of well-educated experts (out of the 48 national groups recruited), that totaled around 4500 in the country.[256][257] Dr. Jacques Pépin, a Quebecer author of The Origins of AIDS, stipulates that Haiti was one of HIV's entry points to the United States and that one of them may have carried HIV back across the Atlantic in the 1960s.[257] Although the virus may have been present in the United States as early as 1966,[258] the vast majority of infections occurring outside sub-Saharan Africa (including the U.S.) can be traced back to a single unknown individual who became infected with HIV in Haiti and then brought the infection to the United States at some time around 1969.[259] The epidemic then rapidly spread among high-risk groups (initially, sexually promiscuous men who have sex with men). By 1978, the prevalence of HIV-1 among homosexual male residents of New York City and San Francisco was estimated at 5%, suggesting that several thousand individuals in the country had been infected.[259]
Society and culture
Stigma
AIDS stigma exists around the world in a variety of ways, including ostracism, rejection, discrimination and avoidance of HIV-infected people; compulsory HIV testing without prior consent or protection of confidentiality; violence against HIV-infected individuals or people who are perceived to be infected with HIV; and the quarantine of HIV-infected individuals.[20] Stigma-related violence or the fear of violence prevents many people from seeking HIV testing, returning for their results, or securing treatment, possibly turning what could be a manageable chronic illness into a death sentence and perpetuating the spread of HIV.[261]
AIDS stigma has been further divided into the following three categories:
- Instrumental AIDS stigma—a reflection of the fear and apprehension that are likely to be associated with any deadly and transmissible illness.[262]
- Symbolic AIDS stigma—the use of HIV/AIDS to express attitudes toward the social groups or lifestyles perceived to be associated with the disease.[262]
- Courtesy AIDS stigma—stigmatization of people connected to the issue of HIV/AIDS or HIV-positive people.[263]
Often, AIDS stigma is expressed in conjunction with one or more other stigmas, particularly those associated with homosexuality, bisexuality, promiscuity, prostitution, and intravenous drug use.[264]
In many developed countries, there is an association between AIDS and homosexuality or bisexuality, and this association is correlated with higher levels of sexual prejudice, such as anti-homosexual or anti-bisexual attitudes.[265] There is also a perceived association between AIDS and all male-male sexual behavior, including sex between uninfected men.[262] However, the dominant mode of spread worldwide for HIV remains heterosexual transmission.[266]
In 2003, as part of an overall reform of marriage and population legislation, it became legal for people with AIDS to marry in China.[267]
In 2013, the U.S. National Library of Medicine developed a traveling exhibition titled Surviving and Thriving: AIDS, Politics, and Culture;[268] this covered medical research, the U.S. government's response, and personal stories from people with AIDS, caregivers, and activists.[269]
Economic impact
HIV/AIDS affects the economics of both individuals and countries.[221] The gross domestic product of the most affected countries has decreased due to the lack of human capital.[221][270] Without proper nutrition, health care and medicine, large numbers of people die from AIDS-related complications. Before death they will not only be unable to work, but will also require significant medical care. It is estimated that as of 2007 there were 12 million AIDS orphans.[221] Many are cared for by elderly grandparents.[271]
Returning to work after beginning treatment for HIV/AIDS is difficult, and affected people often work less than the average worker. Unemployment in people with HIV/AIDS also is associated with suicidal ideation, memory problems, and social isolation. Employment increases self-esteem, sense of dignity, confidence, and quality of life for people with HIV/AIDS. Anti-retroviral treatment may help people with HIV/AIDS work more, and may increase the chance that a person with HIV/AIDS will be employed (low-quality evidence).[272]
By affecting mainly young adults, AIDS reduces the taxable population, in turn reducing the resources available for public expenditures such as education and health services not related to AIDS, resulting in increasing pressure on the state's finances and slower growth of the economy. This causes a slower growth of the tax base, an effect that is reinforced if there are growing expenditures on treating the sick, training (to replace sick workers), sick pay and caring for AIDS orphans. This is especially true if the sharp increase in adult mortality shifts the responsibility from the family to the government in caring for these orphans.[271]
At the household level, AIDS causes both loss of income and increased spending on healthcare. A study in Côte d'Ivoire showed that households having a person with HIV/AIDS spent twice as much on medical expenses as other households. This additional expenditure also leaves less income to spend on education and other personal or family investment.[273]
Religion and AIDS
The topic of religion and AIDS has become highly controversial, primarily because some religious authorities have publicly declared their opposition to the use of condoms.[274][275] The religious approach to prevent the spread of AIDS, according to a report by American health expert Matthew Hanley titled The Catholic Church and the Global AIDS Crisis, argues that cultural changes are needed, including a re-emphasis on fidelity within marriage and sexual abstinence outside of it.[275]
Some religious organizations have claimed that prayer can cure HIV/AIDS. In 2011, the BBC reported that some churches in London were claiming that prayer would cure AIDS, and the Hackney-based Centre for the Study of Sexual Health and HIV reported that several people stopped taking their medication, sometimes on the direct advice of their pastor, leading to a number of deaths.[276] The Synagogue Church Of All Nations advertised an "anointing water" to promote God's healing, although the group denies advising people to stop taking medication.[276]
Media portrayal
One of the first high-profile cases of AIDS was the American Rock Hudson, a gay actor who had been married and divorced earlier in life, who died on October 2, 1985, having announced that he was suffering from the virus on July 25 that year. He had been diagnosed during 1984.[277] A notable British casualty of AIDS that year was Nicholas Eden, a gay politician and son of the late prime minister Anthony Eden.[278] On November 24, 1991, the virus claimed the life of British rock star Freddie Mercury, lead singer of the band Queen, who died from an AIDS-related illness having only revealed the diagnosis on the previous day.[279] However, he had been diagnosed as HIV-positive in 1987. One of the first high-profile heterosexual cases of the virus was American tennis player Arthur Ashe. He was diagnosed as HIV-positive on August 31, 1988, having contracted the virus from blood transfusions during heart surgery earlier in the 1980s. Further tests within 24 hours of the initial diagnosis revealed that Ashe had AIDS, but he did not tell the public about his diagnosis until April 1992.[280] He died as a result on February 6, 1993, aged 49.[281]
Therese Frare's photograph of gay activist David Kirby, as he lay dying from AIDS while surrounded by family, was taken in April 1990. Life magazine said the photo became the one image "most powerfully identified with the HIV/AIDS epidemic." The photo was displayed in Life, was the winner of the World Press Photo, and acquired worldwide notoriety after being used in a United Colors of Benetton advertising campaign in 1992.[282]
Criminal transmission
Criminal transmission of HIV is the intentional or reckless infection of a person with the human immunodeficiency virus (HIV). Some countries or jurisdictions, including some areas of the United States, have laws that criminalize HIV transmission or exposure.[283] Others may charge the accused under laws enacted before the HIV pandemic.
In 1996, Ugandan-born Canadian Johnson Aziga was diagnosed with HIV; he subsequently had unprotected sex with 11 women without disclosing his diagnosis. By 2003, seven had contracted HIV; two died from complications related to AIDS.[284][285] Aziga was convicted of first-degree murder and sentenced to life imprisonment.[286]
Misconceptions
There are many misconceptions about HIV and AIDS. Three of the most common are that AIDS can spread through casual contact, that sexual intercourse with a virgin will cure AIDS,[287][288][289] and that HIV can infect only gay men and drug users. In 2014, some among the British public wrongly thought one could get HIV from kissing (16%), sharing a glass (5%), spitting (16%), a public toilet seat (4%), and coughing or sneezing (5%).[290] Other misconceptions are that any act of anal intercourse between two uninfected gay men can lead to HIV infection, and that open discussion of HIV and homosexuality in schools will lead to increased rates of AIDS.[291][292]
A small group of individuals continue to dispute the connection between HIV and AIDS,[293] the existence of HIV itself, or the validity of HIV testing and treatment methods.[294][295] These claims, known as AIDS denialism, have been examined and rejected by the scientific community.[296] However, they have had a significant political impact, particularly in South Africa, where the government's official embrace of AIDS denialism (1999–2005) was responsible for its ineffective response to that country's AIDS epidemic, and has been blamed for hundreds of thousands of avoidable deaths and HIV infections.[297][298][299]
Several discredited conspiracy theories have held that HIV was created by scientists, either inadvertently or deliberately. Operation INFEKTION was a worldwide Soviet active measures operation to spread the claim that the United States had created HIV/AIDS. Surveys show that a significant number of people believed—and continue to believe—in such claims.[300]
Research
HIV/AIDS research includes all medical research which attempts to prevent, treat, or cure HIV/AIDS, along with fundamental research about the nature of HIV as an infectious agent, and about AIDS as the disease caused by HIV.
Many governments and research institutions participate in HIV/AIDS research. This research includes behavioral health interventions such as sex education, and drug development, such as research into microbicides for sexually transmitted diseases, HIV vaccines, and antiretroviral drugs. Other medical research areas include the topics of pre-exposure prophylaxis, post-exposure prophylaxis, and circumcision and HIV. Public health officials, researchers, and programs can gain a more comprehensive picture of the barriers they face, and the efficacy of current approaches to HIV treatment and prevention, by tracking standard HIV indicators.[301] Use of common indicators is an increasing focus of development organizations and researchers.[302][303]
References
- ^ a b c d "What Are HIV and AIDS? | HIV.gov". www.hiv.gov. U.S. Department of Health and Human Services (HHS). May 15, 2017. Archived from the original on September 22, 2019. Retrieved September 10,2017.
- ^ "HIV Classification: CDC and WHO Staging Systems | AIDS Education and Training Centers National Coordinating Resource Center (AETC NCRC)". aidsetc.org. AIDS Education and Training Center Program. Archived from the original on October 18, 2017. Retrieved September 10,2017.
- ^ "Wear your red ribbon this World AIDS Day | UNAIDS". www.unaids.org. UNAIDS Secretariat. Archivedfrom the original on September 10, 2017. Retrieved September 10,2017.
- ^ a b c d e f g h i j k l m"HIV/AIDS Fact sheet N°360". World Health Organization. November 2015. Archived from the original on February 17, 2016. Retrieved February 11, 2016.
- ^ a b c d e "About HIV/AIDS". CDC. December 6, 2015. Archived from the original on February 24, 2016. Retrieved February 11, 2016.
- ^ a b c UNAIDS (May 18, 2012). "The quest for an HIV vaccine". Archived from the original on May 24, 2012.
- ^ a b c UNAIDS, World Health Organization (December 2007). "2007 AIDS epidemic update" (PDF). Archived from the original (PDF) on May 27, 2008. Retrieved March 12, 2008.
- ^ a b c d e "Global HIV & AIDS statistics — 2019 fact sheet". www.unaids.org. UNAIDS. Archived from the original on December 4, 2019. Retrieved December 21, 2019.
- ^ Sepkowitz KA (June 2001). "AIDS – the first 20 years". The New England Journal of Medicine. 344(23): 1764–72. doi:10.1056/NEJM200106073442306. PMID 11396444.
- ^ Krämer A, Kretzschmar M, Krickeberg K (2010). Modern infectious disease epidemiology concepts, methods, mathematical models, and public health (Online-Ausg. ed.). New York: Springer. p. 88. ISBN 978-0-387-93835-6. Archived from the original on September 24, 2015. Retrieved June 27, 2015.
- ^ Kirch W (2008). Encyclopedia of Public Health. New York: Springer. pp. 676–77. ISBN 978-1-4020-5613-0. Archived from the original on September 11, 2015. Retrieved June 27,2015.
- ^ a b c d e f g h i Rom WN, Markowitz SB, eds. (2007). Environmental and occupational medicine (4th ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. p. 745. ISBN 978-0-7817-6299-1. Archived from the original on September 11, 2015. Retrieved June 27,2015.
- ^ "HIV and Its Transmission". Centers for Disease Control and Prevention. 2003. Archived from the original on February 4, 2005. Retrieved May 23,2006.
- ^ "Retrovirus Definition". AIDSinfo. Archived from the original on December 28, 2019. Retrieved December 28, 2019.
- ^ a b Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV (PDF). World Health Organization. 2015. p. 13. ISBN 978-92-4-150956-5. Archived(PDF) from the original on October 14, 2015.
- ^ "Fact Sheet - World AIDS Day 2019"(PDF). www.unaids.org. Archived (PDF) from the original on December 21, 2019. Retrieved December 21, 2019.
- ^ a b Kallings LO (March 2008). "The first postmodern pandemic: 25 years of HIV/AIDS". Journal of Internal Medicine. 263 (3): 218–43. doi:10.1111/j.1365-2796.2007.01910.x. PMID 18205765.(subscription required)
- ^ a b Sharp PM, Hahn BH (September 2011). "Origins of HIV and the AIDS pandemic". Cold Spring Harbor Perspectives in Medicine. 1 (1): a006841. doi:10.1101/cshperspect.a006841. PMC 3234451. PMID 22229120.
- ^ Gallo RC (October 2006). "A reflection on HIV/AIDS research after 25 years". Retrovirology. 3 (1): 72. doi:10.1186/1742-4690-3-72. PMC 1629027. PMID 17054781.
- ^ a b c "The impact of AIDS on people and societies" (PDF). 2006 Report on the global AIDS epidemic. UNAIDS. 2006. ISBN 978-92-9173-479-5.
- ^ Endersby, Jim (2016). "Myth Busters". Science. 351 (6268): 35. Bibcode:2016Sci...351...35E. doi:10.1126/science.aad2891. Archived from the original on February 22, 2016. Retrieved February 14, 2016.
- ^ McCullom, Rob (February 26, 2013). "An African Pope Won't Change the Vatican's Views on Condoms and AIDS". The Atlantic. Archived from the original on March 8, 2016. Retrieved February 14,2016.
- ^ Harden, Victoria Angela (2012). AIDS at 30: A History. Potomac Books Inc. p. 324. ISBN 978-1-59797-294-9.
- ^ a b c d e f Mandell, Bennett, and Dolan (2010). Chapter 121.
- ^ a b c d e f g h i j k l m n op WHO case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related disease in adults and children (PDF). Geneva: World Health Organization. 2007. pp. 6–16. ISBN 978-92-4-159562-9. Archived(PDF) from the original on October 31, 2013.
- ^ Diseases and disorders. Tarrytown, NY: Marshall Cavendish. 2008. p. 25. ISBN 978-0-7614-7771-6. Archivedfrom the original on September 19, 2015. Retrieved June 27, 2015.
- ^ a b c d e f g h i j k l m n oMandell, Bennett, and Dolan (2010). Chapter 118.
- ^ a b c d e f g h i j k l m n op q r Vogel M, Schwarze-Zander C, Wasmuth JC, Spengler U, Sauerbruch T, Rockstroh JK (July 2010). "The treatment of patients with HIV". Deutsches Arzteblatt International. 107 (28–29): 507–15, quiz 516. doi:10.3238/arztebl.2010.0507. PMC 2915483. PMID 20703338.
- ^ Evian, Clive (2006). Primary HIV/AIDS care: a practical guide for primary health care personnel in a clinical and supportive setting (Updated 4th ed.). Houghton [South Africa]: Jacana. p. 29. ISBN 978-1-77009-198-6. Archived from the original on September 11, 2015. Retrieved June 27,2015.
- ^ Charles B. Hicks, MD (2001). Jacques W.A.J. Reeders & Philip Charles Goodman (ed.). Radiology of AIDS. Berlin [u.a.]: Springer. p. 19. ISBN 978-3-540-66510-6. Archived from the original on May 9, 2016. Retrieved June 27,2015.
- ^ Elliott, Tom (2012). Lecture Notes: Medical Microbiology and Infection. John Wiley & Sons. p. 273. ISBN 978-1-118-37226-5. Archived from the original on September 19, 2015. Retrieved June 27,2015.
- ^ a b Blankson JN (March 2010). "Control of HIV-1 replication in elite suppressors". Discovery Medicine. 9 (46): 261–66. PMID 20350494.
- ^ Walker BD (August–September 2007). "Elite control of HIV Infection: implications for vaccines and treatment". Topics in HIV Medicine. 15 (4): 134–36. PMID 17720999.
- ^ Holmes CB, Losina E, Walensky RP, Yazdanpanah Y, Freedberg KA (March 2003). "Review of human immunodeficiency virus type 1-related opportunistic infections in sub-Saharan Africa". Clinical Infectious Diseases. 36 (5): 652–62. doi:10.1086/367655. PMID 12594648.
- ^ Chu C, Selwyn PA (February 2011). "Complications of HIV infection: a systems-based approach". American Family Physician. 83 (4): 395–406. PMID 21322514.
- ^ a b c d e Mandell, Bennett, and Dolan (2010). Chapter 169.
- ^ Mittal R, Rath S, Vemuganti GK (July 2013). "Ocular surface squamous neoplasia – Review of etio-pathogenesis and an update on clinico-pathological diagnosis". Saudi Journal of Ophthalmology. 27 (3): 177–86. doi:10.1016/j.sjopt.2013.07.002. PMC 3770226. PMID 24227983.
- ^ "AIDS". MedlinePlus. A.D.A.M. Archived from the original on June 18, 2012. Retrieved June 14,2012.
- ^ Sestak K (July 2005). "Chronic diarrhea and AIDS: insights into studies with non-human primates". Current HIV Research. 3 (3): 199–205. doi:10.2174/1570162054368084. PMID 16022653.
- ^ Murray ED, Buttner N, Price BH (2012). "Depression and Psychosis in Neurological Practice". In Bradley WG, Daroff RB, Fenichel GM, Jankovic J (eds.). Bradley's Neurology in Clinical Practice: Expert Consult – Online and Print, 6e (Bradley, Neurology in Clinical Practice e-dition 2v Set). 1 (6th ed.). Philadelphia: Elsevier/Saunders. p. 101. ISBN 978-1-4377-0434-1.
- ^ a b Donegan, Elizabeth; Stuart, Maria; Niland, Joyce C.; Sacks, Henry S.; Azen, Stanley P.; Dietrich, Shelby L.; Faucett, Cheryl; Fletcher, Mary Ann; Kleinman, Steven H.; Operskalski, Eva A.; Perkins, Herbert A.; Pindyck, Johanna; Schiff, Eugene R.; Stites, Daniel P.; Tomasulo, Peter A.; Mosley, James W. (November 15, 1990). "Infection with Human Immunodeficiency Virus Type 1 (HIV-1) among Recipients of Antibody-Positive Blood Donations". Annals of Internal Medicine. 113(10): 733–739. doi:10.7326/0003-4819-113-10-733. Retrieved May 11, 2020.
- ^ Coovadia H (2004). "Antiretroviral agents—how best to protect infants from HIV and save their mothers from AIDS". N. Engl. J. Med. 351 (3): 289–292. doi:10.1056/NEJMe048128. PMID 15247337.
- ^ Smith DK, Grohskopf LA, Black RJ, Auerbach JD, Veronese F, Struble KA, Cheever L, Johnson M, Paxton LA, Onorato IM, Greenberg AE (January 21, 2005). "Antiretroviral postexposure prophylaxis after sexual, injection-drug use, or other nonoccupational exposure to HIV in the United States: recommendations from the U.S. Department of Health and Human Services". MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports / Centers for Disease Control. 54 (RR-2): 1–20. PMID 15660015.
- ^ Kripke C (August 1, 2007). "Antiretroviral prophylaxis for occupational exposure to HIV". American Family Physician. 76 (3): 375–6. PMID 17708137.
- ^ a b c d Dosekun O, Fox J (July 2010). "An overview of the relative risks of different sexual behaviours on HIV transmission". Current Opinion in HIV and AIDS. 5 (4): 291–7. doi:10.1097/COH.0b013e32833a88a3. PMID 20543603.
- ^ Cunha, Burke (2012). Antibiotic Essentials 2012 (11 ed.). Jones & Bartlett Publishers. p. 303. ISBN 9781449693831.
- ^ a b Boily MC, Baggaley RF, Wang L, Masse B, White RG, Hayes RJ, Alary M (February 2009). "Heterosexual risk of HIV-1 infection per sexual act: systematic review and meta-analysis of observational studies". The Lancet Infectious Diseases. 9 (2): 118–29. doi:10.1016/S1473-3099(09)70021-0. PMC 4467783. PMID 19179227.
- ^ Baggaley RF, White RG, Boily MC (December 2008). "Systematic review of orogenital HIV-1 transmission probabilities". International Journal of Epidemiology. 37 (6): 1255–65. doi:10.1093/ije/dyn151. PMC 2638872. PMID 18664564.
- ^ a b c Kripke C (August 2007). "Antiretroviral prophylaxis for occupational exposure to HIV". American Family Physician. 76 (3): 375–76. PMID 17708137.
- ^ van der Kuyl AC, Cornelissen M (September 2007). "Identifying HIV-1 dual infections". Retrovirology. 4: 67. doi:10.1186/1742-4690-4-67. PMC 2045676. PMID 17892568.
- ^ McCray, Eugene; Mermin, Jonathan (September 27, 2017). "Dear Colleague: September 27, 2017". Division of HIV/AIDS Prevention. Centers for Disease Control and Prevention. Archivedfrom the original on January 30, 2018. Retrieved February 1,2018.
- ^ LeMessurier, J; Traversy, G; Varsaneux, O; Weekes, M; Avey, MT; Niragira, O; Gervais, R; Guyatt, G; Rodin, R (November 19, 2018). "Risk of sexual transmission of human immunodeficiency virus with antiretroviral therapy, suppressed viral load and condom use: a systematic review". Canadian Medical Association Journal. 190 (46): E1350–E1360. doi:10.1503/cmaj.180311. PMC 6239917. PMID 30455270.
- ^ "HIV and Men". Centers for Disease Control and Prevention. U.S. Department of Health & Human Services. Archived from the original on December 1, 2019. Retrieved November 3, 2019.
- ^ "HIV and Gay and Bisexual Men". Centers for Disease Control and Prevention. U.S. Department of Health & Human Services. Archived from the original on November 2, 2019. Retrieved November 3, 2019.
- ^ a b "HIV Among Gay and Bisexual Men"(PDF). Archived (PDF)from the original on December 18, 2016. Retrieved January 1,2017.
- ^ a b "Today's HIV/AIDS Epidemic Factsheet"(PDF). Centers for Disease Control and Prevention. Archived(PDF) from the original on December 19, 2016. Retrieved December 31,2016.
- ^ a b c d e f g Boily MC, Baggaley RF, Wang L, Masse B, White RG, Hayes RJ, Alary M (February 2009). "Heterosexual risk of HIV-1 infection per sexual act: systematic review and meta-analysis of observational studies". The Lancet. Infectious Diseases. 9 (2): 118–29. doi:10.1016/S1473-3099(09)70021-0. PMC 4467783. PMID 19179227.
- ^ Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, Brookmeyer R (July 2012). "Global epidemiology of HIV infection in men who have sex with men". The Lancet. 380 (9839): 367–77. doi:10.1016/S0140-6736(12)60821-6. PMC 3805037. PMID 22819660.
- ^ Yu M, Vajdy M (August 2010). "Mucosal HIV transmission and vaccination strategies through oral compared with vaginal and rectal routes". Expert Opinion on Biological Therapy. 10(8): 1181–95. doi:10.1517/14712598.2010.496776. PMC 2904634. PMID 20624114.
- ^ Stürchler, Dieter A. (2006). Exposure a guide to sources of infections. Washington, DC: ASM Press. p. 544. ISBN 978-1-55581-376-5. Archived from the original on November 30, 2015. Retrieved June 27,2015.
- ^ Pattman R, et al., eds. (2010). Oxford handbook of genitourinary medicine, HIV, and sexual health(2nd ed.). Oxford: Oxford University Press. p. 95. ISBN 978-0-19-957166-6.
- ^ a b c Dosekun O, Fox J (July 2010). "An overview of the relative risks of different sexual behaviours on HIV transmission". Current Opinion in HIV and AIDS. 5 (4): 291–97. doi:10.1097/COH.0b013e32833a88a3. PMID 20543603.
- ^ a b Ng BE, Butler LM, Horvath T, Rutherford GW (March 2011). Butler LM (ed.). "Population-based biomedical sexually transmitted infection control interventions for reducing HIV infection". The Cochrane Database of Systematic Reviews(3): CD001220. doi:10.1002/14651858.CD001220.pub3. PMID 21412869.
- ^ Anderson J (February 2012). "Women and HIV: motherhood and more". Current Opinion in Infectious Diseases. 25(1): 58–65. doi:10.1097/QCO.0b013e32834ef514. PMID 22156896.
- ^ Kerrigan, Deanna (2012). The Global HIV Epidemics among Sex Workers. World Bank Publications. pp. 1–5. ISBN 978-0-8213-9775-6. Archived from the original on September 19, 2015. Retrieved June 27,2015.
- ^ Aral, Sevgi (2013). The New Public Health and STD/HIV Prevention: Personal, Public and Health Systems Approaches. Springer. p. 120. ISBN 978-1-4614-4526-5. Archived from the original on September 24, 2015. Retrieved June 27, 2015.
- ^ Klimas N, Koneru AO, Fletcher MA (June 2008). "Overview of HIV". Psychosomatic Medicine. 70 (5): 523–30. doi:10.1097/PSY.0b013e31817ae69f. PMID 18541903.
- ^ Draughon JE, Sheridan DJ (2012). "Nonoccupational postexposure prophylaxis following sexual assault in industrialized low-HIV-prevalence countries: a review". Psychology, Health & Medicine. 17 (2): 235–54. doi:10.1080/13548506.2011.579984. PMID 22372741.
- ^ Baggaley RF, Boily MC, White RG, Alary M (April 2006). "Risk of HIV-1 transmission for parenteral exposure and blood transfusion: a systematic review and meta-analysis". AIDS. 20(6): 805–12. doi:10.1097/01.aids.0000218543.46963.6d. PMID 16549963.
- ^ "Needlestick Prevention Guide" (PDF). 2002. pp. 5–6. Archived(PDF) from the original on July 12, 2018. Retrieved November 10, 2019.
- ^ "HIV in the United States: An Overview". Center for Disease Control and Prevention. March 2012. Archived from the original on May 1, 2013.
- ^ "Will I need a blood transfusion?" (PDF). NHS patient information. National Health Services. 2011. Archived (PDF)from the original on October 25, 2012. Retrieved August 29,2012.
- ^ Centers for Disease Control Prevention (CDC) (October 2010). "HIV transmission through transfusion – Missouri and Colorado, 2008". Morbidity and Mortality Weekly Report. 59 (41): 1335–39. PMID 20966896.
- ^ UNAIDS 2011 pg. 60–70
- ^ "Blood safety ... for too few". World Health Organization. 2001. Archived from the original on January 17, 2005.
- ^ Simonds RJ (November 1993). "HIV transmission by organ and tissue transplantation". AIDS. 7 Suppl 2: S35–38. doi:10.1097/00002030-199311002-00008. PMID 8161444.
- ^ a b c Reid SR (August 2009). "Injection drug use, unsafe medical injections, and HIV in Africa: a systematic review". Harm Reduction Journal. 6: 24. doi:10.1186/1477-7517-6-24. PMC 2741434. PMID 19715601.
- ^ a b "Basic Information about HIV and AIDS". Center for Disease Control and Prevention. April 2012. Archivedfrom the original on June 18, 2017.
- ^ Crans, Wayne J. (June 1, 2010). "Why Mosquitoes Cannot Transmit AIDS". rci.rutgers.edu. Rutgers University. New Jersey Agricultural Experiment Station Publication No. H-40101-01-93. Archived from the original on March 29, 2014. Retrieved March 29,2014.
- ^ "Preventing Mother-to-Child Transmission of HIV". HIV.gov. Archived from the original on December 9, 2017. Retrieved December 8, 2017.
- ^ a b c d Coutsoudis A, Kwaan L, Thomson M (October 2010). "Prevention of vertical transmission of HIV-1 in resource-limited settings". Expert Review of Anti-Infective Therapy. 8 (10): 1163–75. doi:10.1586/eri.10.94. PMID 20954881.
- ^ "WHO | Mother-to-child transmission of HIV". WHO. Archived from the original on October 18, 2019. Retrieved December 27, 2019.
- ^ White AB, Mirjahangir JF, Horvath H, Anglemyer A, Read JS (October 2014). "Antiretroviral interventions for preventing breast milk transmission of HIV". The Cochrane Database of Systematic Reviews. 10(10): CD011323. doi:10.1002/14651858.CD011323. PMID 25280769.
- ^ a b c "Infant feeding in the context of HIV". www.who.int. April 2011. Archived from the original on March 9, 2017. Retrieved March 9, 2017.
- ^ Alimonti JB, Ball TB, Fowke KR (July 2003). "Mechanisms of CD4+ T lymphocyte cell death in human immunodeficiency virus infection and AIDS". The Journal of General Virology. 84 (Pt 7): 1649–61. doi:10.1099/vir.0.19110-0. PMID 12810858.
- ^ International Committee on Taxonomy of Viruses(2002). "61.0.6. Lentivirus". National Institutes of Health. Archived from the original on April 18, 2006. Retrieved June 25,2012.
- ^ International Committee on Taxonomy of Viruses (2002). "61. Retroviridae". National Institutes of Health. Archived from the original on December 17, 2001. Retrieved June 25, 2012.
- ^ Levy JA (November 1993). "HIV pathogenesis and long-term survival". AIDS. 7 (11): 1401–10. doi:10.1097/00002030-199311000-00001. PMID 8280406.
- ^ Smith JA, Daniel R (May 2006). "Following the path of the virus: the exploitation of host DNA repair mechanisms by retroviruses". ACS Chemical Biology. 1 (4): 217–26. doi:10.1021/cb600131q. PMID 17163676.
- ^ Martínez MA, ed. (2010). RNA interference and viruses : current innovations and future trends. Norfolk: Caister Academic Press. p. 73. ISBN 978-1-904455-56-1. Archived from the original on September 11, 2015. Retrieved June 27,2015.
- ^ Gerald B. Pier, ed. (2004). Immunology, infection, and immunity. Washington, DC: ASM Press. p. 550. ISBN 978-1-55581-246-1. Archived from the original on May 9, 2016. Retrieved June 27, 2015.
- ^ a b c Zhang C, Zhou S, Groppelli E, Pellegrino P, Williams I, Borrow P, Chain BM, Jolly C (April 2015). "Hybrid spreading mechanisms and T cell activation shape the dynamics of HIV-1 infection". PLOS Computational Biology. 11(4): e1004179. arXiv:1503.08992. Bibcode:2015PLSCB..11E4179Z. doi:10.1371/journal.pcbi.1004179. PMC 4383537. PMID 25837979.
- ^ Jolly C, Kashefi K, Hollinshead M, Sattentau QJ (January 2004). "HIV-1 cell to cell transfer across an Env-induced, actin-dependent synapse". The Journal of Experimental Medicine. 199 (2): 283–93. doi:10.1084/jem.20030648. PMC 2211771. PMID 14734528.
- ^ Sattentau Q (November 2008). "Avoiding the void: cell-to-cell spread of human viruses". Nature Reviews. Microbiology. 6(11): 815–26. doi:10.1038/nrmicro1972. PMID 18923409.
- ^ Sigal A, Kim JT, Balazs AB, Dekel E, Mayo A, Milo R, Baltimore D (August 2011). "Cell-to-cell spread of HIV permits ongoing replication despite antiretroviral therapy". Nature. 477(7362): 95–98. Bibcode:2011Natur.477...95S. doi:10.1038/nature10347. PMID 21849975.
- ^ Gilbert PB, McKeague IW, Eisen G, Mullins C, Guéye-NDiaye A, Mboup S, Kanki PJ (February 2003). "Comparison of HIV-1 and HIV-2 infectivity from a prospective cohort study in Senegal". Statistics in Medicine. 22(4): 573–93. doi:10.1002/sim.1342. PMID 12590415.
- ^ a b Reeves JD, Doms RW (June 2002). "Human immunodeficiency virus type 2". The Journal of General Virology. 83 (Pt 6): 1253–65. doi:10.1099/0022-1317-83-6-1253. PMID 12029140.
- ^ Piatak M, Saag MS, Yang LC, Clark SJ, Kappes JC, Luk KC, Hahn BH, Shaw GM, Lifson JD (March 1993). "High levels of HIV-1 in plasma during all stages of infection determined by competitive PCR". Science. 259 (5102): 1749–54. Bibcode:1993Sci...259.1749P. doi:10.1126/science.8096089. PMID 8096089.
- ^ Pantaleo G, Demarest JF, Schacker T, Vaccarezza M, Cohen OJ, Daucher M, Graziosi C, Schnittman SS, Quinn TC, Shaw GM, Perrin L, Tambussi G, Lazzarin A, Sekaly RP, Soudeyns H, Corey L, Fauci AS (January 1997). "The qualitative nature of the primary immune response to HIV infection is a prognosticator of disease progression independent of the initial level of plasma viremia". Proceedings of the National Academy of Sciences of the United States of America. 94 (1): 254–58. Bibcode:1997PNAS...94..254P. doi:10.1073/pnas.94.1.254. PMC 19306. PMID 8990195.
- ^ Hel Z, McGhee JR, Mestecky J (June 2006). "HIV infection: first battle decides the war". Trends in Immunology. 27 (6): 274–81. doi:10.1016/j.it.2006.04.007. PMID 16679064.
- ^ Pillay, Deenan; Genetti, Anna Maria; Weiss, Robin A. (2007). "Human Immunodeficiency Viruses". In Zuckerman, Arie J.; et al. (eds.). Principles and practice of clinical virology(6th ed.). Hoboken, NJ: Wiley. p. 905. ISBN 978-0-470-51799-4.
- ^ Mehandru S, Poles MA, Tenner-Racz K, Horowitz A, Hurley A, Hogan C, Boden D, Racz P, Markowitz M (September 2004). "Primary HIV-1 infection is associated with preferential depletion of CD4+ T lymphocytes from effector sites in the gastrointestinal tract". The Journal of Experimental Medicine. 200 (6): 761–70. doi:10.1084/jem.20041196. PMC 2211967. PMID 15365095.
- ^ Brenchley JM, Schacker TW, Ruff LE, Price DA, Taylor JH, Beilman GJ, Nguyen PL, Khoruts A, Larson M, Haase AT, Douek DC (September 2004). "CD4+ T cell depletion during all stages of HIV disease occurs predominantly in the gastrointestinal tract". The Journal of Experimental Medicine. 200 (6): 749–59. doi:10.1084/jem.20040874. PMC 2211962. PMID 15365096.
- ^ Olson WC, Jacobson JM (March 2009). "CCR5 monoclonal antibodies for HIV-1 therapy". Current Opinion in HIV and AIDS. 4 (2): 104–11. doi:10.1097/COH.0b013e3283224015. PMC 2760828. PMID 19339948.
- ^ a b editor, Julio Aliberti (2011). Control of Innate and Adaptive Immune Responses During Infectious Diseases. New York: Springer Verlag. p. 145. ISBN 978-1-4614-0483-5. Archived from the original on September 24, 2015. Retrieved June 27,2015.
- ^ Appay V, Sauce D (January 2008). "Immune activation and inflammation in HIV-1 infection: causes and consequences". The Journal of Pathology. 214(2): 231–41. doi:10.1002/path.2276. PMID 18161758.
- ^ Brenchley JM, Price DA, Schacker TW, Asher TE, Silvestri G, Rao S, Kazzaz Z, Bornstein E, Lambotte O, Altmann D, Blazar BR, Rodriguez B, Teixeira-Johnson L, Landay A, Martin JN, Hecht FM, Picker LJ, Lederman MM, Deeks SG, Douek DC (December 2006). "Microbial translocation is a cause of systemic immune activation in chronic HIV infection". Nature Medicine. 12 (12): 1365–71. doi:10.1038/nm1511. PMC 1717013. PMID 17115046.
- ^ "HIV/AIDS Testing". CDC. March 16, 2018. Archived from the original on April 14, 2018. Retrieved April 14, 2018.
- ^ a b US Preventive Services Task, Force.; Owens, DK; Davidson, KW; Krist, AH; Barry, MJ; Cabana, M; Caughey, AB; Curry, SJ; Doubeni, CA; Epling JW, Jr; Kubik, M; Landefeld, CS; Mangione, CM; Pbert, L; Silverstein, M; Simon, MA; Tseng, CW; Wong, JB (June 18, 2019). "Screening for HIV Infection: US Preventive Services Task Force Recommendation Statement". JAMA. 321(23): 2326–2336. doi:10.1001/jama.2019.6587. PMID 31184701.
- ^ a b Kellerman S, Essajee S (July 2010). "HIV testing for children in resource-limited settings: what are we waiting for?". PLOS Medicine. 7 (7): e1000285. doi:10.1371/journal.pmed.1000285. PMC 2907270. PMID 20652012.
- ^ a b c UNAIDS 2011 pg. 70–80
- ^ a b c Schneider E, Whitmore S, Glynn KM, Dominguez K, Mitsch A, McKenna MT (December 2008). "Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years – United States, 2008". MMWR. Recommendations and Reports. 57 (RR-10): 1–12. PMID 19052530.
- ^ a b c Centers for Disease Control Prevention (CDC) (April 2014). "Revised surveillance case definition for HIV infection – United States, 2014". MMWR. Recommendations and Reports. 63 (RR-03): 1–10. PMID 24717910.
- ^ Crosby R, Bounse S (March 2012). "Condom effectiveness: where are we now?". Sexual Health. 9 (1): 10–17. doi:10.1071/SH11036. PMID 22348628.
- ^ "Condom Facts and Figures". World Health Organization. August 2003. Archived from the original on October 18, 2012. Retrieved January 17, 2006.
- ^ Gallo MF, Kilbourne-Brook M, Coffey PS (March 2012). "A review of the effectiveness and acceptability of the female condom for dual protection". Sexual Health. 9 (1): 18–26. doi:10.1071/SH11037. PMID 22348629.
- ^ a b Celum C, Baeten JM (February 2012). "Tenofovir-based pre-exposure prophylaxis for HIV prevention: evolving evidence". Current Opinion in Infectious Diseases. 25 (1): 51–57. doi:10.1097/QCO.0b013e32834ef5ef. PMC 3266126. PMID 22156901.
- ^ Baptista M, Ramalho-Santos J (November 2009). "Spermicides, microbicides and antiviral agents: recent advances in the development of novel multi-functional compounds". Mini Reviews in Medicinal Chemistry. 9 (13): 1556–67. doi:10.2174/138955709790361548. PMID 20205637.
- ^ Siegfried N, Muller M, Deeks JJ, Volmink J (April 2009). Siegfried N (ed.). "Male circumcision for prevention of heterosexual acquisition of HIV in men". The Cochrane Database of Systematic Reviews (2): CD003362. doi:10.1002/14651858.CD003362.pub2. PMID 19370585.
- ^ "WHO and UNAIDS announce recommendations from expert consultation on male circumcision for HIV prevention". World Health Organization. March 28, 2007. Archived from the original on July 3, 2011.
- ^ Larke N (May 27, 2010). "Male circumcision, HIV and sexually transmitted infections: a review". British Journal of Nursing. 19 (10): 629–34. doi:10.12968/bjon.2010.19.10.48201. PMC 3836228. PMID 20622758.
- ^ Eaton L, Kalichman SC (November 2009). "Behavioral aspects of male circumcision for the prevention of HIV infection". Current HIV/AIDS Reports. 6 (4): 187–93. doi:10.1007/s11904-009-0025-9. PMC 3557929. PMID 19849961.(subscription required)
- ^ Kim HH, Li PS, Goldstein M (November 2010). "Male circumcision: Africa and beyond?". Current Opinion in Urology. 20(6): 515–19. doi:10.1097/MOU.0b013e32833f1b21. PMID 20844437.
- ^ Templeton DJ, Millett GA, Grulich AE (February 2010). "Male circumcision to reduce the risk of HIV and sexually transmitted infections among men who have sex with men". Current Opinion in Infectious Diseases. 23(1): 45–52. doi:10.1097/QCO.0b013e328334e54d. PMID 19935420.
- ^ Wiysonge CS, Kongnyuy EJ, Shey M, Muula AS, Navti OB, Akl EA, Lo YR (June 2011). Wiysonge CS (ed.). "Male circumcision for prevention of homosexual acquisition of HIV in men". The Cochrane Database of Systematic Reviews (6): CD007496. doi:10.1002/14651858.CD007496.pub2. PMID 21678366.
- ^ a b Marrazzo JM, del Rio C, Holtgrave DR, Cohen MS, Kalichman SC, Mayer KH, Montaner JS, Wheeler DP, Grant RM, Grinsztejn B, Kumarasamy N, Shoptaw S, Walensky RP, Dabis F, Sugarman J, Benson CA (July 23–30, 2014). "HIV prevention in clinical care settings: 2014 recommendations of the International Antiviral Society–USA Panel". JAMA. 312 (4): 390–409. doi:10.1001/jama.2014.7999. PMC 6309682. PMID 25038358.
- ^ Eaton LA, Kalichman S (December 2007). "Risk compensation in HIV prevention: implications for vaccines, microbicides, and other biomedical HIV prevention technologies". Current HIV/AIDS Reports. 4 (4): 165–72. doi:10.1007/s11904-007-0024-7. PMC 2937204. PMID 18366947.
- ^ Underhill K, Operario D, Montgomery P (October 2007). Operario D (ed.). "Abstinence-only programs for HIV infection prevention in high-income countries". The Cochrane Database of Systematic Reviews (4): CD005421. doi:10.1002/14651858.CD005421.pub2. PMID 17943855. Archived from the original on November 25, 2010. Retrieved May 31, 2012.
- ^ Tolli MV (October 2012). "Effectiveness of peer education interventions for HIV prevention, adolescent pregnancy prevention and sexual health promotion for young people: a systematic review of European studies". Health Education Research. 27(5): 904–13. doi:10.1093/her/cys055. PMID 22641791.
- ^ Ljubojević S, Lipozenčić J (2010). "Sexually transmitted infections and adolescence". Acta Dermatovenerologica Croatica. 18 (4): 305–10. PMID 21251451.
- ^ International technical guidance on sexuality education: an evidence-informed approach(PDF). Paris: UNESCO. 2018. p. 12. ISBN 978-92-3-100259-5. Archived(PDF) from the original on November 13, 2018. Retrieved February 22,2018.
- ^ Patel VL, Yoskowitz NA, Kaufman DR, Shortliffe EH (September 2008). "Discerning patterns of human immunodeficiency virus risk in healthy young adults". The American Journal of Medicine. 121(9): 758–64. doi:10.1016/j.amjmed.2008.04.022. PMC 2597652. PMID 18724961.
- ^ Fonner VA, Denison J, Kennedy CE, O'Reilly K, Sweat M (September 2012). "Voluntary counseling and testing (VCT) for changing HIV-related risk behavior in developing countries". The Cochrane Database of Systematic Reviews. 9(9): CD001224. doi:10.1002/14651858.CD001224.pub4. PMC 3931252. PMID 22972050.
- ^ Lopez, LM; Grey, TW; Chen, M; Denison, J; Stuart, G (August 9, 2016). "Behavioral interventions for improving contraceptive use among women living with HIV". The Cochrane Database of Systematic Reviews (8): CD010243. doi:10.1002/14651858.CD010243.pub3. PMC 7092487. PMID 27505053.
- ^ a b Anglemyer A, Rutherford GW, Horvath T, Baggaley RC, Egger M, Siegfried N (April 2013). "Antiretroviral therapy for prevention of HIV transmission in HIV-discordant couples". The Cochrane Database of Systematic Reviews. 4(4): CD009153. doi:10.1002/14651858.CD009153.pub3. PMC 4026368. PMID 23633367.
- ^ Chou R, Selph S, Dana T, Bougatsos C, Zakher B, Blazina I, Korthuis PT (November 2012). "Screening for HIV: systematic review to update the 2005 U.S. Preventive Services Task Force recommendation". Annals of Internal Medicine. 157 (10): 706–18. doi:10.7326/0003-4819-157-10-201211200-00007. PMID 23165662.
- ^ Owens, Douglas K.; Davidson, Karina W.; Krist, Alex H.; Barry, Michael J.; Cabana, Michael; Caughey, Aaron B.; Curry, Susan J.; Doubeni, Chyke A.; Epling, John W.; Kubik, Martha; Landefeld, C. Seth; Mangione, Carol M.; Pbert, Lori; Silverstein, Michael; Simon, Melissa A.; Tseng, Chien-Wen; Wong, John B. (June 11, 2019). "Preexposure Prophylaxis for the Prevention of HIV Infection". JAMA. 321(22): 2203–2213. doi:10.1001/jama.2019.6390. PMID 31184747.
- ^ Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, Chiamwongpaet S, Kitisin P, Natrujirote P, Kittimunkong S, Chuachoowong R, Gvetadze RJ, McNicholl JM, Paxton LA, Curlin ME, Hendrix CW, Vanichseni S (June 2013). "Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial". The Lancet. 381(9883): 2083–90. doi:10.1016/S0140-6736(13)61127-7. PMID 23769234.
- ^ US Preventive Services Task, Force.; Owens, DK; Davidson, KW; Krist, AH; Barry, MJ; Cabana, M; Caughey, AB; Curry, SJ; Doubeni, CA; Epling JW, Jr; Kubik, M; Landefeld, CS; Mangione, CM; Pbert, L; Silverstein, M; Simon, MA; Tseng, CW; Wong, JB (June 11, 2019). "Preexposure Prophylaxis for the Prevention of HIV Infection: US Preventive Services Task Force Recommendation Statement". JAMA. 321(22): 2203–2213. doi:10.1001/jama.2019.6390. PMID 31184747.
- ^ Centers for Disease Control (CDC) (August 1987). "Recommendations for prevention of HIV transmission in health-care settings". MMWR Supplements. 36 (2): 1S–18S. PMID 3112554. Archived from the original on July 9, 2017.
- ^ a b Kurth AE, Celum C, Baeten JM, Vermund SH, Wasserheit JN (March 2011). "Combination HIV prevention: significance, challenges, and opportunities". Current HIV/AIDS Reports. 8 (1): 62–72. doi:10.1007/s11904-010-0063-3. PMC 3036787. PMID 20941553.
- ^ MacArthur GJ, Minozzi S, Martin N, Vickerman P, Deren S, Bruneau J, Degenhardt L, Hickman M (October 2012). "Opiate substitution treatment and HIV transmission in people who inject drugs: systematic review and meta-analysis". BMJ. 345 (oct03 3): e5945. doi:10.1136/bmj.e5945. PMC 3489107. PMID 23038795.
- ^ a b "HIV exposure through contact with body fluids". Prescrire International. 21 (126): 100–01, 103–05. April 2012. PMID 22515138.
- ^ Kuhar DT, Henderson DK, Struble KA, Heneine W, Thomas V, Cheever LW, Gomaa A, Panlilio AL (September 2013). "Updated US Public Health Service guidelines for the management of occupational exposures to human immunodeficiency virus and recommendations for postexposure prophylaxis". Infection Control and Hospital Epidemiology. 34 (9): 875–92. doi:10.1086/672271. PMID 23917901.
- ^ Linden JA (September 2011). "Clinical practice. Care of the adult patient after sexual assault". The New England Journal of Medicine. 365 (9): 834–41. doi:10.1056/NEJMcp1102869. PMID 21879901.
- ^ Young TN, Arens FJ, Kennedy GE, Laurie JW, Rutherford GW (January 2007). Young T (ed.). "Antiretroviral post-exposure prophylaxis (PEP) for occupational HIV exposure". The Cochrane Database of Systematic Reviews (1): CD002835. doi:10.1002/14651858.CD002835.pub3. PMID 17253483.
- ^ Siegfried N, van der Merwe L, Brocklehurst P, Sint TT (July 2011). Siegfried N (ed.). "Antiretrovirals for reducing the risk of mother-to-child transmission of HIV infection". The Cochrane Database of Systematic Reviews (7): CD003510. doi:10.1002/14651858.CD003510.pub3. PMID 21735394.
- ^ "WHO HIV and Infant Feeding Technical Consultation Held on behalf of the Inter-agency Task Team (IATT) on Prevention of HIV – Infections in Pregnant Women, Mothers and their Infants – Consensus statement" (PDF). October 25–27, 2006. Archived (PDF) from the original on April 9, 2008. Retrieved March 12, 2008.
- ^ Horvath T, Madi BC, Iuppa IM, Kennedy GE, Rutherford G, Read JS (January 2009). Horvath T (ed.). "Interventions for preventing late postnatal mother-to-child transmission of HIV". The Cochrane Database of Systematic Reviews (1): CD006734. doi:10.1002/14651858.CD006734.pub2. PMID 19160297.
- ^ "WHO validates elimination of mother-to-child transmission of HIV and syphilis in Cuba". World Health Organization. June 30, 2015. Archived from the original on September 4, 2015. Retrieved August 30, 2015.
- ^ Reynell L, Trkola A (March 2012). "HIV vaccines: an attainable goal?". Swiss Medical Weekly. 142: w13535. doi:10.4414/smw.2012.13535. PMID 22389197.
- ^ U.S. Army Office of the Surgeon General (March 21, 2011). "HIV Vaccine Trial in Thai Adults". ClinicalTrials.gov. Archived from the original on October 19, 2011. Retrieved June 28,2011.
- ^ U.S. Army Office of the Surgeon General (June 2, 2010). "Follow up of Thai Adult Volunteers With Breakthrough HIV Infection After Participation in a Preventive HIV Vaccine Trial". ClinicalTrials.gov. Archived from the original on June 9, 2012.
- ^ May MT, Ingle SM (December 2011). "Life expectancy of HIV-positive adults: a review". Sexual Health. 8 (4): 526–33. doi:10.1071/SH11046. PMID 22127039.
- ^ a b UNAIDS 2011 pg. 1–10
- ^ Davis, Nicola (March 8, 2020). "Second Person Ever to Be Cleared of HIV Reveals Identity". The Guardian. Retrieved March 8, 2020.
- ^ a b c d Antiretroviral therapy for HIV infection in adults and adolescents: recommendations for a public health approach(PDF). World Health Organization. 2010. pp. 19–20. ISBN 978-92-4-159976-4. Archived(PDF) from the original on July 9, 2012.
- ^ a b Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection (PDF). World Health Organization. 2013. pp. 28–30. ISBN 978-92-4-150572-7. Archived(PDF) from the original on February 9, 2014.
- ^ "UPDATE OF RECOMMENDATIONS ON FIRST- AND SECOND-LINE ANTIRETROVIRAL REGIMENS" (PDF). World Health Organization. July 2019. Retrieved November 16,2019.
- ^ "Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents" (PDF). Department of Health and Human Services. February 12, 2013. p. i. Archived (PDF) from the original on November 1, 2016. Retrieved January 3, 2014.
- ^ Sterne JA, May M, Costagliola D, de Wolf F, Phillips AN, Harris R, Funk MJ, Geskus RB, Gill J, Dabis F, Miró JM, Justice AC, Ledergerber B, Fätkenheuer G, Hogg RS, Monforte AD, Saag M, Smith C, Staszewski S, Egger M, Cole SR (April 2009). "Timing of initiation of antiretroviral therapy in AIDS-free HIV-1-infected patients: a collaborative analysis of 18 HIV cohort studies". The Lancet. 373 (9672): 1352–63. doi:10.1016/S0140-6736(09)60612-7. PMC 2670965. PMID 19361855.
- ^ Beard J, Feeley F, Rosen S (November 2009). "Economic and quality of life outcomes of antiretroviral therapy for HIV/AIDS in developing countries: a systematic literature review". AIDS Care. 21 (11): 1343–56. doi:10.1080/09540120902889926. PMID 20024710.
- ^ Attia S, Egger M, Müller M, Zwahlen M, Low N (July 2009). "Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis". AIDS. 23 (11): 1397–404. doi:10.1097/QAD.0b013e32832b7dca. PMID 19381076.
- ^ Orrell C (November 2005). "Antiretroviral adherence in a resource-poor setting". Current HIV/AIDS Reports. 2 (4): 171–76. doi:10.1007/s11904-005-0012-8. PMID 16343374.
- ^ Malta M, Strathdee SA, Magnanini MM, Bastos FI (August 2008). "Adherence to antiretroviral therapy for human immunodeficiency virus/acquired immune deficiency syndrome among drug users: a systematic review". Addiction. 103 (8): 1242–57. doi:10.1111/j.1360-0443.2008.02269.x. PMID 18855813.
- ^ Nachega JB, Marconi VC, van Zyl GU, Gardner EM, Preiser W, Hong SY, Mills EJ, Gross R (April 2011). "HIV treatment adherence, drug resistance, virologic failure: evolving concepts". Infectious Disorders Drug Targets. 11 (2): 167–74. doi:10.2174/187152611795589663. PMC 5072419. PMID 21406048.
- ^ Orsi F, d'Almeida C (May 2010). "Soaring antiretroviral prices, TRIPS and TRIPS flexibilities: a burning issue for antiretroviral treatment scale-up in developing countries". Current Opinion in HIV and AIDS. 5 (3): 237–41. doi:10.1097/COH.0b013e32833860ba. PMID 20539080.
- ^ Nachega JB, Mills EJ, Schechter M (January 2010). "Antiretroviral therapy adherence and retention in care in middle-income and low-income countries: current status of knowledge and research priorities". Current Opinion in HIV and AIDS. 5 (1): 70–77. doi:10.1097/COH.0b013e328333ad61. PMID 20046150.
- ^ a b c Montessori V, Press N, Harris M, Akagi L, Montaner JS (January 2004). "Adverse effects of antiretroviral therapy for HIV infection". Canadian Medical Association Journal. 170(2): 229–38. PMC 315530. PMID 14734438.
- ^ a b c Burgoyne RW, Tan DH (March 2008). "Prolongation and quality of life for HIV-infected adults treated with highly active antiretroviral therapy (HAART): a balancing act". Journal of Antimicrobial Chemotherapy. 61 (3): 469–73. doi:10.1093/jac/dkm499. PMID 18174196.
- ^ Barbaro G, Barbarini G (December 2011). "Human immunodeficiency virus & cardiovascular risk". The Indian Journal of Medical Research. 134(6): 898–903. doi:10.4103/0971-5916.92634. PMC 3284097. PMID 22310821.
- ^ "Summary of recommendations on when to start ART in children" (PDF). Consolidated ARV guidelines, June 2013. June 2013. Archived(PDF) from the original on October 18, 2014.
- ^ "Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection" (PDF). Department of Health and Human Services, February 2014. March 2014. Archived (PDF)from the original on September 14, 2015.
- ^ "Guidelines for intensified tuberculosis case-finding and isoniazid preventive therapy for people living with HIV in resource-constrained settings" (PDF). Department of HIV/AIDS, World Health Organization 2011. 2011. Archived (PDF) from the original on October 19, 2014.
- ^ Laurence J (January 2006). "Hepatitis A and B virus immunization in HIV-infected persons". The AIDS Reader. 16 (1): 15–17. PMID 16433468.
- ^ a b UNAIDS 2011 pg. 150–160
- ^ Huang L, Cattamanchi A, Davis JL, den Boon S, Kovacs J, Meshnick S, Miller RF, Walzer PD, Worodria W, Masur H (June 2011). "HIV-associated Pneumocystis pneumonia". Proceedings of the American Thoracic Society. 8 (3): 294–300. doi:10.1513/pats.201009-062WR. PMC 3132788. PMID 21653531.
- ^ "Treating opportunistic infections among HIV-infected adults and adolescents. Recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association/Infectious Diseases Society of America". Department of Health and Human Services. February 2, 2007. Archived from the original on July 27, 2018. Retrieved July 26,2018.
- ^ a b Smith, Blaine T., ed. (2008). Concepts in immunology and immunotherapeutics(4th ed.). Bethesda, MD: American Society of Health-System Pharmacists. p. 143. ISBN 978-1-58528-127-5. Archived from the original on November 28, 2015. Retrieved June 27,2015.
- ^ Beck CR, McKenzie BC, Hashim AB, Harris RC, Zanuzdana A, Agboado G, et al. (September 2013). "Influenza vaccination for immunocompromised patients: summary of a systematic review and meta-analysis". Influenza and Other Respiratory Viruses. 7 Suppl 2: 72–75. doi:10.1111/irv.12084. PMC 5909396. PMID 24034488.
- ^ Lee KY, Tsai MS, Kuo KC, Tsai JC, Sun HY, Cheng AC, Chang SY, Lee CH, Hung CC (2014). "Pneumococcal vaccination among HIV-infected adult patients in the era of combination antiretroviral therapy". Human Vaccines & Immunotherapeutics. 10(12): 3700–10. doi:10.4161/hv.32247. PMC 4514044. PMID 25483681.
- ^ a b World Health Organization (May 2003). Nutrient requirements for people living with HIV/AIDS: Report of a technical consultation(PDF). Geneva. Archived (PDF) from the original on March 25, 2009. Retrieved March 31, 2009.
- ^ Forrester JE, Sztam KA (December 2011). "Micronutrients in HIV/AIDS: is there evidence to change the WHO 2003 recommendations?". The American Journal of Clinical Nutrition. 94 (6): 1683S–1689S. doi:10.3945/ajcn.111.011999. PMC 3226021. PMID 22089440.
- ^ Nunnari G, Coco C, Pinzone MR, Pavone P, Berretta M, Di Rosa M, Schnell M, Calabrese G, Cacopardo B (June 2012). "The role of micronutrients in the diet of HIV-1-infected individuals". Frontiers in Bioscience. 4 (7): 2442–56. doi:10.2741/e556. PMID 22652651. Archived from the original on April 16, 2015.
- ^ Zeng L, Zhang L (December 2011). "Efficacy and safety of zinc supplementation for adults, children and pregnant women with HIV infection: systematic review". Tropical Medicine & International Health. 16(12): 1474–82. doi:10.1111/j.1365-3156.2011.02871.x. PMID 21895892.
- ^ Visser ME, Durao S, Sinclair D, Irlam JH, Siegfried N (May 2017). "Micronutrient supplementation in adults with HIV infection". The Cochrane Database of Systematic Reviews. 5: CD003650. doi:10.1002/14651858.CD003650.pub4. PMC 5458097. PMID 28518221.
- ^ Stone CA, Kawai K, Kupka R, Fawzi WW (November 2010). "Role of selenium in HIV infection". Nutrition Reviews. 68 (11): 671–81. doi:10.1111/j.1753-4887.2010.00337.x. PMC 3066516. PMID 20961297.
- ^ a b Siegfried N, Irlam JH, Visser ME, Rollins NN (March 2012). "Micronutrient supplementation in pregnant women with HIV infection". The Cochrane Database of Systematic Reviews (3): CD009755. doi:10.1002/14651858.CD009755. PMID 22419344.
- ^ Irlam JH, Siegfried N, Visser ME, Rollins NC (October 2013). "Micronutrient supplementation for children with HIV infection". The Cochrane Database of Systematic Reviews (10): CD010666. doi:10.1002/14651858.CD010666. PMID 24114375.
- ^ Littlewood RA, Vanable PA (September 2008). "Complementary and alternative medicine use among HIV-positive people: research synthesis and implications for HIV care". AIDS Care. 20 (8): 1002–18. doi:10.1080/09540120701767216. PMC 2570227. PMID 18608078.
- ^ Mills E, Wu P, Ernst E (June 2005). "Complementary therapies for the treatment of HIV: in search of the evidence". International Journal of STD & AIDS. 16 (6): 395–403. doi:10.1258/0956462054093962. PMID 15969772.
- ^ Liu JP, Manheimer E, Yang M (July 2005). Liu JP (ed.). "Herbal medicines for treating HIV infection and AIDS". The Cochrane Database of Systematic Reviews (3): CD003937. doi:10.1002/14651858.CD003937.pub2. PMID 16034917.
- ^ Lutge EE, Gray A, Siegfried N (April 2013). "The medical use of cannabis for reducing morbidity and mortality in patients with HIV/AIDS". The Cochrane Database of Systematic Reviews. 4(4): CD005175. doi:10.1002/14651858.CD005175.pub3. PMID 23633327.
- ^ a b c Knoll B, Lassmann B, Temesgen Z (December 2007). "Current status of HIV infection: a review for non-HIV-treating physicians". International Journal of Dermatology. 46 (12): 1219–28. doi:10.1111/j.1365-4632.2007.03520.x. PMID 18173512.
- ^ a b Morgan D, Mahe C, Mayanja B, Okongo JM, Lubega R, Whitworth JA (March 2002). "HIV-1 infection in rural Africa: is there a difference in median time to AIDS and survival compared with that in industrialized countries?". AIDS. 16(4): 597–603. doi:10.1097/00002030-200203080-00011. PMID 11873003.
- ^ Zwahlen M, Egger M (2006). "Progression and mortality of untreated HIV-positive individuals living in resource-limited settings: update of literature review and evidence synthesis"(PDF). UNAIDS Obligation HQ/05/422204. Archived (PDF) from the original on April 9, 2008. Retrieved March 19, 2008.
- ^ a b Antiretroviral Therapy Cohort Collaboration (July 2008). "Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies". The Lancet. 372 (9635): 293–99. doi:10.1016/S0140-6736(08)61113-7. PMC 3130543. PMID 18657708.
- ^ Schackman BR, Gebo KA, Walensky RP, Losina E, Muccio T, Sax PE, Weinstein MC, Seage GR, Moore RD, Freedberg KA (November 2006). "The lifetime cost of current human immunodeficiency virus care in the United States". Medical Care. 44 (11): 990–97. doi:10.1097/01.mlr.0000228021.89490.2a. PMID 17063130.
- ^ van Sighem AI, Gras LA, Reiss P, Brinkman K, de Wolf F (June 2010). "Life expectancy of recently diagnosed asymptomatic HIV-infected patients approaches that of uninfected individuals". AIDS. 24 (10): 1527–35. doi:10.1097/QAD.0b013e32833a3946. PMID 20467289.
- ^ a b Cheung MC, Pantanowitz L, Dezube BJ (June–July 2005). "AIDS-related malignancies: emerging challenges in the era of highly active antiretroviral therapy". The Oncologist. 10 (6): 412–26. CiteSeerX 10.1.1.561.4760. doi:10.1634/theoncologist.10-6-412. PMID 15967835.
- ^ Tang J, Kaslow RA (2003). "The impact of host genetics on HIV infection and disease progression in the era of highly active antiretroviral therapy". AIDS. 17 Suppl 4 (Suppl 4): S51–60. doi:10.1097/00002030-200317004-00006. PMID 15080180.
- ^ Lawn SD (January 2004). "AIDS in Africa: the impact of coinfections on the pathogenesis of HIV-1 infection". The Journal of Infection. 48(1): 1–12. doi:10.1016/j.jinf.2003.09.001. PMID 14667787.
- ^ Campbell GR, Pasquier E, Watkins J, Bourgarel-Rey V, Peyrot V, Esquieu D, Barbier P, de Mareuil J, Braguer D, Kaleebu P, Yirrell DL, Loret EP (November 2004). "The glutamine-rich region of the HIV-1 Tat protein is involved in T-cell apoptosis". The Journal of Biological Chemistry. 279(46): 48197–204. doi:10.1074/jbc.M406195200. PMID 15331610.
- ^ Campbell GR, Watkins JD, Esquieu D, Pasquier E, Loret EP, Spector SA (November 2005). "The C terminus of HIV-1 Tat modulates the extent of CD178-mediated apoptosis of T cells". The Journal of Biological Chemistry. 280 (46): 38376–82. doi:10.1074/jbc.M506630200. PMID 16155003.
- ^ "Tuberculosis". Fact sheet 104. World Health Organization. March 2012. Archived from the original on August 23, 2012. Retrieved August 29, 2012.
- ^ World Health Organization (2011). Global tuberculosis control 2011 (PDF). ISBN 978-92-4-156438-0. Archived from the original (PDF) on September 6, 2012. Retrieved August 29,2012.
- ^ Rubin R, Strayer DS, Rubin E, eds. (2011). Rubin's pathology: clinicopathologic foundations of medicine(Sixth ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 154. ISBN 978-1-60547-968-2. Archived from the original on September 24, 2015. Retrieved June 27,2015.
- ^ Nelson VM, Benson AB (January 2017). "Epidemiology of Anal Canal Cancer". Surgical Oncology Clinics of North America. 26 (1): 9–15. doi:10.1016/j.soc.2016.07.001. PMID 27889039.
- ^ Woods SP, Moore DJ, Weber E, Grant I (June 2009). "Cognitive neuropsychology of HIV-associated neurocognitive disorders". Neuropsychology Review. 19 (2): 152–68. doi:10.1007/s11065-009-9102-5. PMC 2690857. PMID 19462243.
- ^ Brown TT, Qaqish RB (November 2006). "Antiretroviral therapy and the prevalence of osteopenia and osteoporosis: a meta-analytic review". AIDS. 20(17): 2165–74. doi:10.1097/QAD.0b013e32801022eb. PMID 17086056.
- ^ Nicholas PK, Kemppainen JK, Canaval GE, Corless IB, Sefcik EF, Nokes KM, Bain CA, Kirksey KM, Eller LS, Dole PJ, Hamilton MJ, Coleman CL, Holzemer WL, Reynolds NR, Portillo CJ, Bunch EH, Wantland DJ, Voss J, Phillips R, Tsai YF, Mendez MR, Lindgren TG, Davis SM, Gallagher DM (February 2007). "Symptom management and self-care for peripheral neuropathy in HIV/AIDS". AIDS Care. 19 (2): 179–89. doi:10.1080/09540120600971083. PMID 17364396.
- ^ Boshoff C, Weiss R (May 2002). "AIDS-related malignancies". Nature Reviews. Cancer. 2 (5): 373–82. doi:10.1038/nrc797. PMID 12044013.
- ^ Yarchoan R, Tosato G, Little RF (August 2005). "Therapy insight: AIDS-related malignancies – the influence of antiviral therapy on pathogenesis and management". Nature Clinical Practice Oncology. 2 (8): 406–15, quiz 423. doi:10.1038/ncponc0253. PMID 16130937.
- ^ Post FA, Holt SG (February 2009). "Recent developments in HIV and the kidney". Current Opinion in Infectious Diseases. 22 (1): 43–48. doi:10.1097/QCO.0b013e328320ffec. PMID 19106702.
- ^ a b Roser, Max; Ritchie, Hannah (April 3, 2018). "HIV / AIDS". Our World in Data. Archivedfrom the original on October 4, 2019. Retrieved October 4,2019.
- ^ Cohen MS, Hellmann N, Levy JA, DeCock K, Lange J (April 2008). "The spread, treatment, and prevention of HIV-1: evolution of a global pandemic". The Journal of Clinical Investigation. 118 (4): 1244–54. doi:10.1172/JCI34706. PMC 2276790. PMID 18382737.
- ^ a b c "Fact sheet – Latest statistics on the status of the AIDS epidemic | UNAIDS". www.unaids.org. Archived from the original on July 13, 2017. Retrieved July 21, 2017.
- ^ "UNAIDS reports a 52% reduction in new HIV infections among children and a combined 33% reduction among adults and children since 2001". UNAIDS. Archived from the original on October 1, 2013. Retrieved October 7, 2013.
- ^ a b c d UNAIDS 2011 pg. 20–30
- ^ a b c UNAIDS 2011 pp. 40–50
- ^ a b c d Mandell, Bennett, and Dolan (2010). Chapter 117.
- ^ New HIV infections among children have been reduced by 50% or more in seven countries in sub-Saharan AfricaArchived June 30, 2013, at the Wayback Machine, UN AIDS, Geneva, June 25, 2013.
- ^ Centers for Disease Control Prevention (CDC) (June 2011). "HIV surveillance – United States, 1981–2008". Morbidity and Mortality Weekly Report. 60 (21): 689–93. PMID 21637182.
- ^ Public Health England (2016). HIV in the United Kingdom: 2016 Report(PDF). Archived (PDF)from the original on April 25, 2017.
- ^ Surveillance; riques, Risk Assessment Division = Le VIH et le sida au Canada: rapport de surveillance en date du 31 décembre 2009 / Division de la surveillance et de l'évaluation des (2010). HIV and AIDS in Canada: surveillance report to December 31, 2009 (PDF). Ottawa: Public Health Agency of Canada, Centre for Communicable Diseases and Infection Control, Surveillance and Risk Assessment Division. ISBN 978-1-100-52141-1. Archived from the original (PDF) on January 19, 2012.
- ^ "Global Report Fact Sheet" (PDF). UNAIDS. 2010. Archived from the original (PDF)on March 19, 2013.
- ^ "Country Comparison :: HIV/AIDS – Adult Prevalence Rate". CIA World Factbook. Archived from the original on December 21, 2014. Retrieved November 6, 2014.
- ^ "How I told the world about Aids". BBC News. June 5, 2006. Archived from the original on February 12, 2019. Retrieved February 12, 2019.
- ^ Gottlieb MS (June 2006). "Pneumocystis pneumonia – Los Angeles. 1981". American Journal of Public Health. 96 (6): 980–81, discussion 982–83. doi:10.2105/AJPH.96.6.980. PMC 1470612. PMID 16714472. Archived from the original on April 22, 2009.
- ^ Friedman-Kien AE (October 1981). "Disseminated Kaposi's sarcoma syndrome in young homosexual men". Journal of the American Academy of Dermatology. 5 (4): 468–71. doi:10.1016/S0190-9622(81)80010-2. PMID 7287964.
- ^ Hymes KB, Cheung T, Greene JB, Prose NS, Marcus A, Ballard H, William DC, Laubenstein LJ (September 1981). "Kaposi's sarcoma in homosexual men-a report of eight cases". The Lancet. 2 (8247): 598–600. doi:10.1016/S0140-6736(81)92740-9. PMID 6116083.
- ^ a b Basavapathruni A, Anderson KS (December 2007). "Reverse transcription of the HIV-1 pandemic". FASEB Journal. 21 (14): 3795–808. doi:10.1096/fj.07-8697rev. PMID 17639073.
- ^ Centers for Disease Control (CDC) (May 1982). "Persistent, generalized lymphadenopathy among homosexual males". Morbidity and Mortality Weekly Report. 31 (19): 249–51. PMID 6808340. Archived from the original on October 18, 2011.
- ^ Barré-Sinoussi F, Chermann JC, Rey F, Nugeyre MT, Chamaret S, Gruest J, Dauguet C, Axler-Blin C, Vézinet-Brun F, Rouzioux C, Rozenbaum W, Montagnier L (May 1983). "Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS)". Science. 220(4599): 868–71. Bibcode:1983Sci...220..868B. doi:10.1126/science.6189183. PMID 6189183.
- ^ a b Centers for Disease Control (CDC) (July 1982). "Opportunistic infections and Kaposi's sarcoma among Haitians in the United States". Morbidity and Mortality Weekly Report. 31 (26): 353–54, 360–61. PMID 6811853. Archived from the original on September 20, 2011.
- ^ Gilman, Sander L (1987). Gilman, Sander L. (ed.). "AIDS and Syphilis: The Iconography of Disease". October. 43: 87–107. doi:10.2307/3397566. JSTOR 3397566.
- ^ "Making Headway Under Hellacious Circumstances" (PDF). American Association for the Advancement of Science. July 28, 2006. Archived (PDF) from the original on June 24, 2008. Retrieved June 23,2008.
- ^ Altman LK (May 11, 1982). "New homosexual disorder worries health officials". The New York Times. Archived from the original on April 30, 2013. Retrieved August 31, 2011.
- ^ Kher U (July 27, 1982). "A Name for the Plague". Time. Archived from the original on March 7, 2008. Retrieved March 10,2008.
- ^ Centers for Disease Control (CDC) (September 1982). "Update on acquired immune deficiency syndrome (AIDS) – United States". Morbidity and Mortality Weekly Report. 31 (37): 507–08, 513–14. PMID 6815471.
- ^ Gallo RC, Sarin PS, Gelmann EP, Robert-Guroff M, Richardson E, Kalyanaraman VS, Mann D, Sidhu GD, Stahl RE, Zolla-Pazner S, Leibowitch J, Popovic M (May 1983). "Isolation of human T-cell leukemia virus in acquired immune deficiency syndrome (AIDS)". Science. 220(4599): 865–67. Bibcode:1983Sci...220..865G. doi:10.1126/science.6601823. PMID 6601823.
- ^ Barré-Sinoussi F, Chermann JC, Rey F, Nugeyre MT, Chamaret S, Gruest J, Dauguet C, Axler-Blin C, Vézinet-Brun F, Rouzioux C, Rozenbaum W, Montagnier L (May 1983). "Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS)". Science. 220(4599): 868–71. Bibcode:1983Sci...220..868B. doi:10.1126/science.6189183. PMID 6189183.
- ^ Aldrich R, Wotherspoon G, eds. (2001). Who's who in gay and lesbian history. London: Routledge. p. 154. ISBN 978-0-415-22974-6. Archived from the original on September 11, 2015. Retrieved June 27,2015.
- ^ Gao F, Bailes E, Robertson DL, Chen Y, Rodenburg CM, Michael SF, Cummins LB, Arthur LO, Peeters M, Shaw GM, Sharp PM, Hahn BH (February 1999). "Origin of HIV-1 in the chimpanzee Pan troglodytes troglodytes". Nature. 397 (6718): 436–41. Bibcode:1999Natur.397..436G. doi:10.1038/17130. PMID 9989410.
- ^ Keele BF, Van Heuverswyn F, Li Y, Bailes E, Takehisa J, Santiago ML, Bibollet-Ruche F, Chen Y, Wain LV, Liegeois F, Loul S, Ngole EM, Bienvenue Y, Delaporte E, Brookfield JF, Sharp PM, Shaw GM, Peeters M, Hahn BH (July 2006). "Chimpanzee reservoirs of pandemic and nonpandemic HIV-1". Science. 313(5786): 523–26. Bibcode:2006Sci...313..523K. doi:10.1126/science.1126531. PMC 2442710. PMID 16728595.
- ^ Goodier JL, Kazazian HH (October 2008). "Retrotransposons revisited: the restraint and rehabilitation of parasites". Cell. 135 (1): 23–35. doi:10.1016/j.cell.2008.09.022. PMID 18854152.(subscription required)
- ^ Sharp PM, Bailes E, Chaudhuri RR, Rodenburg CM, Santiago MO, Hahn BH (June 2001). "The origins of acquired immune deficiency syndrome viruses: where and when?". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 356 (1410): 867–76. doi:10.1098/rstb.2001.0863. PMC 1088480. PMID 11405934.
- ^ Kalish ML, Wolfe ND, Ndongmo CB, McNicholl J, Robbins KE, Aidoo M, Fonjungo PN, Alemnji G, Zeh C, Djoko CF, Mpoudi-Ngole E, Burke DS, Folks TM (December 2005). "Central African hunters exposed to simian immunodeficiency virus". Emerging Infectious Diseases. 11(12): 1928–30. doi:10.3201/eid1112.050394. PMC 3367631. PMID 16485481.
- ^ a b Marx PA, Alcabes PG, Drucker E (June 2001). "Serial human passage of simian immunodeficiency virus by unsterile injections and the emergence of epidemic human immunodeficiency virus in Africa". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 356 (1410): 911–20. doi:10.1098/rstb.2001.0867. PMC 1088484. PMID 11405938.
- ^ Worobey M, Gemmel M, Teuwen DE, Haselkorn T, Kunstman K, Bunce M, Muyembe JJ, Kabongo JM, Kalengayi RM, Van Marck E, Gilbert MT, Wolinsky SM (October 2008). "Direct evidence of extensive diversity of HIV-1 in Kinshasa by 1960". Nature. 455 (7213): 661–64. Bibcode:2008Natur.455..661W. doi:10.1038/nature07390. PMC 3682493. PMID 18833279.(subscription required)
- ^ a b de Sousa JD, Müller V, Lemey P, Vandamme AM (April 2010). Martin DP (ed.). "High GUD incidence in the early 20th century created a particularly permissive time window for the origin and initial spread of epidemic HIV strains". PLOS One. 5 (4): e9936. Bibcode:2010PLoSO...5.9936S. doi:10.1371/journal.pone.0009936. PMC 2848574. PMID 20376191.
- ^ Chitnis A, Rawls D, Moore J (January 2000). "Origin of HIV type 1 in colonial French Equatorial Africa?". AIDS Research and Human Retroviruses. 16 (1): 5–8. doi:10.1089/088922200309548. PMID 10628811.(subscription required)
- ^ Donald G. McNeil, Jr.(September 16, 2010). "Precursor to H.I.V. Was in Monkeys for Millennia". The New York Times. Archivedfrom the original on May 11, 2011. Retrieved September 17, 2010.
Dr. Marx believes that the crucial event was the introduction into Africa of millions of inexpensive, mass-produced syringes in the 1950s. ... suspect that the growth of colonial cities is to blame. Before 1910, no Central African town had more than 10,000 people. But urban migration rose, increasing sexual contacts and leading to red-light districts.
- ^ Zhu T, Korber BT, Nahmias AJ, Hooper E, Sharp PM, Ho DD (February 1998). "An African HIV-1 sequence from 1959 and implications for the origin of the epidemic". Nature. 391 (6667): 594–97. Bibcode:1998Natur.391..594Z. doi:10.1038/35400. PMID 9468138.
- ^ Lederberg J, ed. (2000). Encyclopedia of Microbiology (2nd ed.). Burlington, MA: Elsevier. p. 106. ISBN 978-0-08-054848-7. Archivedfrom the original on September 10, 2017. Retrieved December 12,2016.
- ^ Jackson, Regine O., ed. (2011). Geographies of the Haitian Diaspora. Routledge. p. 12. ISBN 978-0-415-88708-3. Archived from the original on May 9, 2016. Retrieved March 13,2016.
- ^ a b Pépin, Jacques (2011). The Origin of Aids. Cambridge University Press. p. 188. ISBN 978-0-521-18637-7. Archived from the original on May 9, 2016. Retrieved March 13,2016.
- ^ Kolata, Gina (October 28, 1987). "Boy's 1969 Death Suggests AIDS Invaded U.S. Several Times". The New York Times. Archived from the original on February 11, 2009. Retrieved February 11, 2009.
- ^ a b Gilbert MT, Rambaut A, Wlasiuk G, Spira TJ, Pitchenik AE, Worobey M (November 2007). "The emergence of HIV/AIDS in the Americas and beyond" (PDF). Proceedings of the National Academy of Sciences of the United States of America. 104(47): 18566–70. Bibcode:2007PNAS..10418566G. doi:10.1073/pnas.0705329104. PMC 2141817. PMID 17978186. Archived (PDF) from the original on September 24, 2015.
- ^ "Ryan White, an American AIDS Victim". Encyclopædia Britannica. November 7, 2013. Archived from the original on July 22, 2015. Retrieved July 16, 2015.
- ^ Ogden J, Nyblade L (2005). "Common at its core: HIV-related stigma across contexts"(PDF). International Center for Research on Women. Archived from the original (PDF) on February 17, 2007. Retrieved February 15,2007.
- ^ a b c Herek GM, Capitanio JP (1999). "AIDS Stigma and sexual prejudice" (PDF). American Behavioral Scientist. 42 (7): 1130–47. doi:10.1177/0002764299042007006. Archived from the original (PDF)on April 9, 2006. Retrieved March 27,2006.
- ^ Snyder M, Omoto AM, Crain AL (1999). "Punished for their good deeds: stigmatization for AIDS volunteers". American Behavioral Scientist. 42 (7): 1175–92. doi:10.1177/0002764299042007009.
- ^ Sharma, A.K. (2012). Population and society. New Delhi: Concept Pub. Co. p. 242. ISBN 978-81-8069-818-7. Archivedfrom the original on September 24, 2015. Retrieved June 27, 2015.
- ^ Herek GM, Capitanio JP, Widaman KF (March 2002). "HIV-related stigma and knowledge in the United States: prevalence and trends, 1991–1999". American Journal of Public Health. 92 (3): 371–77. doi:10.2105/AJPH.92.3.371. PMC 1447082. PMID 11867313.
- ^ De Cock KM, Jaffe HW, Curran JW (June 2012). "The evolving epidemiology of HIV/AIDS". AIDS. 26 (10): 1205–13. doi:10.1097/QAD.0b013e328354622a. PMID 22706007.
- ^ Richard Spencer (August 21, 2003). "China relaxes laws on love and marriage". The Telegraph. Archivedfrom the original on November 8, 2013. Retrieved October 24,2013.
- ^ "Exhibition – Surviving and Thriving – NLM Exhibition Program". www.nlm.nih.gov. U.S. National Institutes of Health, National Library of Medicine. Archivedfrom the original on December 1, 2017. Retrieved March 16,2018.
- ^ Geiling, Natasha (December 4, 2013). "The Confusing and At-Times Counterproductive 1980s Response to the AIDS Epidemic". Smithsonian.com. Archived from the original on March 16, 2018. Retrieved March 16, 2018.
- ^ Bell C, Devarajan S, Gersbach H (2003). "The long-run economic costs of AIDS: theory and an application to South Africa". World Bank Policy Research Working Paper No. 3152. Archived from the original (PDF)on June 5, 2013. Retrieved April 28, 2008.
- ^ a b Greener R (2002). "AIDS and macroeconomic impact" (PDF). In Forsyth S (ed.). State of The Art: AIDS and Economics. IAEN. pp. 49–55. Archived(PDF) from the original on October 12, 2012.
- ^ Robinson R, Okpo E, Mngoma N (May 2015). "Interventions for improving employment outcomes for workers with HIV". The Cochrane Database of Systematic Reviews. 5 (5): CD010090. doi:10.1002/14651858.CD010090.pub2. hdl:2164/6021. PMID 26022149.
- ^ Over M (1992). "The macroeconomic impact of AIDS in Sub-Saharan Africa, Population and Human Resources Department" (PDF). World Bank. Archived(PDF) from the original on May 27, 2008. Retrieved May 3, 2008.
- ^ "AIDS Stigma". News-medical.net. December 7, 2009. Archived from the original on November 12, 2011. Retrieved November 1, 2011.
- ^ a b "Thirty years after AIDS discovery, appreciation growing for Catholic approach". Catholicnewsagency.com. June 5, 2011. Archivedfrom the original on October 16, 2011. Retrieved November 1,2011.
- ^ a b "Church HIV prayer cure claims 'cause three deaths'". BBC News. October 18, 2011. Archived from the original on October 18, 2011. Retrieved October 18, 2011.
- ^ "Rock Hudson announces he has AIDS – History.com This Day in History – 7/25/1985". History.com. Archivedfrom the original on December 27, 2011. Retrieved November 1,2011.
- ^ Coleman, Brian (June 25, 2007). "Thatcher the gay icon". New Statesman. Archivedfrom the original on November 14, 2011. Retrieved November 1,2011.
- ^ "November 24, 1991: Giant of rock dies". BBC On This Day. BBC News. November 24, 1991. Archived from the original on October 21, 2011. Retrieved November 1, 2011.
- ^ Bliss, Dominic. "Frozen In Time: Arthur Ashe". iTENNISstore.com. Archived from the original on July 30, 2013. Retrieved June 25,2012.
- ^ "Tributes to Arthur Ashe". The Independent. London. February 8, 1993. Archived from the original on November 11, 2012. Retrieved July 24,2012.
- ^ Cosgrove, Ben. "Behind the Picture: The Photo That Changed the Face of AIDS". LIFE magazine. Archived from the original on August 14, 2012. Retrieved August 16, 2012.
- ^ "HIV-Specific Criminal Laws". cdc.gov. June 30, 2014. Archivedfrom the original on October 31, 2014. Retrieved November 22,2014.
- ^ "Aziga found guilty of first-degree murder". CTV.ca News. Archivedfrom the original on October 29, 2013. Retrieved April 9, 2013.
- ^ "HIV killer ruled dangerous offender". CBC News. Archivedfrom the original on September 3, 2012. Retrieved April 9, 2013.
- ^ "A fraudster, not a murderer". National Post. March 30, 2010. Archived from the original on May 15, 2016. Retrieved April 9,2013.
- ^ "'Virgin cure': Three women killed to 'cure' Aids". International Herald Tribune. February 28, 2013. Archivedfrom the original on October 15, 2013. Retrieved September 14,2013.
- ^ Jenny, Carole (2010). Child Abuse and Neglect: Diagnosis, Treatment and Evidence – Expert Consult. Elsevier Health Sciences. p. 187. ISBN 978-1-4377-3621-2. Archived from the original on November 27, 2015. Retrieved June 27,2015.
- ^ Klot, Jennifer; Monica Kathina Juma (2011). HIV/AIDS, Gender, Human Security and Violence in Southern Africa. Pretoria: Africa Institute of South Africa. p. 47. ISBN 978-0-7983-0253-1. Archived from the original on April 26, 2016. Retrieved June 27,2015.
- ^ "HIV Public Knowledge and Attitudes 2014"(PDF). National AIDS Trust. November 2014. p. 9. Archived from the original (PDF) on February 12, 2015. Retrieved February 12,2015.
- ^ Blechner MJ (1997). Hope and mortality: psychodynamic approaches to AIDS and HIV. Hillsdale, NJ: Analytic Press. ISBN 978-0-88163-223-1.
- ^ Kirby DB, Laris BA, Rolleri LA (March 2007). "Sex and HIV education programs: their impact on sexual behaviors of young people throughout the world". The Journal of Adolescent Health. 40 (3): 206–17. doi:10.1016/j.jadohealth.2006.11.143. PMID 17321420.
- ^ Duesberg P (July 1988). "HIV is not the cause of AIDS". Science. 241 (4865): 514, 517. Bibcode:1988Sci...241..514D. doi:10.1126/science.3399880. PMID 3399880.Cohen J (December 1994). "The Duesberg phenomenon" (PDF). Science. 266 (5191): 1642–44. Bibcode:1994Sci...266.1642C. doi:10.1126/science.7992043. PMID 7992043. Archived from the original (PDF) on January 1, 2007.
- ^ Kalichman, Seth (2009). Denying AIDS: Conspiracy Theories, Pseudoscience, and Human Tragedy. New York: Copernicus Books (Springer Science+Business Media). ISBN 978-0-387-79475-4.
- ^ Smith TC, Novella SP (August 2007). "HIV denial in the Internet era". PLOS Medicine. 4(8): e256. doi:10.1371/journal.pmed.0040256. PMC 1949841. PMID 17713982.
- ^ Various (January 14, 2010). "Resources and Links, HIV-AIDS Connection". National Institute of Allergy and Infectious Diseases. Archived from the original on April 7, 2010. Retrieved February 22,2009.
- ^ Watson J (January 2006). "Scientists, activists sue South Africa's AIDS 'denialists'". Nature Medicine. 12 (1): 6. doi:10.1038/nm0106-6a. PMID 16397537.
- ^ Baleta A (March 2003). "S Africa's AIDS activists accuse government of murder". The Lancet. 361(9363): 1105. doi:10.1016/S0140-6736(03)12909-1. PMID 12672319.
- ^ Cohen J (June 2000). "South Africa's new enemy". Science. 288(5474): 2168–70. doi:10.1126/science.288.5474.2168. PMID 10896606.
- ^ Boghardt, Thomas (2009). "Operation INFEKTION Soviet Bloc Intelligence and Its AIDS Disinformation Campaign". Central Intelligence Agency. Archived from the original on May 14, 2011.
- ^ "Indicators – Program Evaluation – CDC". www.cdc.gov. Archivedfrom the original on August 23, 2018. Retrieved August 24,2018.
- ^ "Community-Based Indicators for HIV Programs – MEASURE Evaluation". www.measureevaluation.org. Archived from the original on August 25, 2018. Retrieved August 24, 2018.
- ^ "Data and statistics". World Health Organization. Archivedfrom the original on September 2, 2018. Retrieved August 24,2018.
External links
| Classification | |
|---|---|
| External resources |
| Wikimedia Commons has media related to HIV/AIDS. |
| Wikiquote has quotations related to: HIV/AIDS |
- HIV/AIDS at Curlie
- UNAIDS – Joint United Nations Program on HIV/AIDS.
- AIDSinfo – Information on HIV/AIDS treatment, prevention, and research, U.S. Department of Health and Human Services.
- 2018 Recommendations of the International Antiviral Society
Ebola
| Neem het voorbehoud bij medische informatie in acht. Raadpleeg bij gezondheidsklachten een arts. |
Ebola | ||||
 | ||||
| Coderingen | ||||
| ICD-10 | A98.4 | |||
| ICD-9 | 065.8 | |||
| DiseasesDB | 18043 | |||
| MedlinePlus | 001339 | |||
| eMedicine | med/626 | |||
| MeSH | D019142 | |||
| ||||
Ebola of ebola hemorragische koorts is een bij mensen voorkomende virusziekte die wordt veroorzaakt door het ebolavirus. De ziekte is zeldzaam en komt voor in de vorm van regionale uitbraken in landen in Midden-Afrika. De naam ebola komt van de gelijknamige rivier in Congo (destijds Zaïre) waar in 1976 een tweede uitbraak plaatsvond en ebola voor het eerst door Guido van der Groen en Peter Piot werd herkend en aangetoond in de plaats Yambuku, gelegen op 95 kilometer van de rivier de Ebola.[1][2] De aandoening veroorzaakt een hoog sterftecijfer en er is nog geen specifieke behandeling of geneesmiddel beschikbaar tegen het virus.
Symptomen en ziekteverloop[bewerken | brontekst bewerken]
De incubatieperiode van ebola is 2 tot 21 dagen. Meestal ontwikkelt de patiënt na 7 dagen de eerste ziekteverschijnselen.[3] Nadat de eerste symptomen - koorts, zeer zware hoofdpijn en sterke pijnscheuten - zich voordoen, kan de ziekte snel verergeren. Een atypisch, maar ernstig symptoom is de hik, dat 15% van de patiënten treft.[4]
In het begin van de ziekte zal de patiënt niet-specifieke griepachtige symptomen vertonen, zoals keelpijn, koorts en algemene malaise. Deze symptomen komen snel opzetten en verergeren snel. Hoofd-, spier- en gewrichtspijn, koorts met koude rillingen, geen eetlust en een zwaktegevoel zijn de meest voorkomende vroege symptomen.
Een vlekken vormende huiduitslag vertoont zich soms rond dag vijf van de infectie, voornamelijk op de romp. Deze uitslag is weinig kenmerkend daar het slechts in ongeveer 15% van de gevallen voorkomt. Daarna volgen maag-darmklachten zoals buikpijn, overgeven en diarree. Tekenen van aantasting en bloeding van de slijmvliezen zijn: bindvliesontsteking, moeilijk en pijnlijk slikken en bloedingen op verschillende plaatsen van het maag-darmstelsel. Bloedingen van de slijmvliezen komen in de helft van de gevallen voor. In volgende fases kunnen verdere bloedingen, ontsteking van de hartspier en longoedeem voorkomen.
In de tweede ziekteweek ziet men in de regel het begin van herstel óf een verdere verslechtering met diffuse bloedstolling in de vaten, algeheel orgaanfalen en shock. Wanneer de patiënt aan de infectie overlijdt, gebeurt dit meestal in de tweede week. Herstel duurt lang. Gedurende deze periode ziet men regelmatig complicaties zoals teelbalontsteking, leverontsteking, gewrichtspijn, ontsteking van rug- of beenmerg en oogvliesontsteking.[5]
Besmettingen[bewerken | brontekst bewerken]
Het virus is via alle lichaamssappen overdraagbaar. De versie die in Congo-Kinshasa voorkomt, kan waarschijnlijk via direct contact met de patiënt, door verpleging, of contact met het dode lichaam worden verspreid. Niet iedereen die besmet is met het virus overlijdt hieraan; de mortaliteit ligt naar schatting rond de 50%.[5] Naar alle waarschijnlijkheid spelen individuele factoren zoals de gezondheid en genetische aanleg een rol bij de gevoeligheid voor het virus. Ebola werd voor het eerst wetenschappelijk geregistreerd in 1976. Sinds die uitbraak en tot aan de uitbraak in 2014, zijn er ongeveer twintig verschillende kleinere uitbraken geweest.[6] Tot de uitbraak van de ziekte in 2014 in de West-Afrikaanse landen Guinee en Liberia stierven er per uitbraak enkele honderden mensen. Desalniettemin werd het ebolavirus maandenlang onderwerp van gesprek toen er in 1995 in Congo-Kinshasa weer een uitbraak plaatsvond. Begin 2005 vond een uitbraak van ebola plaats in Etoumbi.
Vleermuizen zijn de waarschijnlijkste bron voor filovirussen. De virussen zijn aangetroffen in verschillende vleermuissoorten die in Afrika leven. Zij verspreiden het virus onder meer via hun ontlasting. Verschillende dieren in het Afrikaanse tropische regenwoud kunnen met het virus worden besmet, zoals chimpansees, gorilla's en antilopen. Als mensen deze dieren slachten en eten, kunnen zij het virus ook krijgen.[7] Rond Meliandou, het dorp van de eerste patiënt in Guinee, worden vleermuizen gegeten.
Het virus lijkt langere tijd te kunnen overleven in de mannelijke geslachtscellen: bij besmette mannen waren maanden na de besmetting (in een geval zelfs na 565 dagen) nog virussen in het sperma aangetroffen. Er zijn dan ook personen besmet na geslachtsgemeenschap met een van ebola genezen man.[8][9]
Epidemieën[bewerken | brontekst bewerken]
1976[bewerken | brontekst bewerken]
De eerste gedocumenteerde epidemieën hebben zich in 1976 in Soedan en Zaïre voorgedaan.[2]
Soedan[bewerken | brontekst bewerken]
In de periode juni tot en met november 1976 brak een ebola-epidemie in de steden Nzara, Maridi, Tembura en Djoeba in het zuiden van Soedan uit. De uitbraak begon in een katoenfabriek in Nzara waar de eerste patiënt op 27 juni 1976 ziek werd, die is op 6 juli gestorven. Collega's van deze patiënt werden ook ziek, waarna de ziekte zich verspreidde over familieleden en gezondheidswerkers. De epidemie verspreidde zich in augustus sterk in een ziekenhuis in Maridi. De verzorging van de zieken speelden hierbij waarschijnlijk een rol. Omdat ook veel personeel ziek werd brak er paniek onder de patiënten en het aanwezige personeel uit, zodat het ziekenhuis voor een groot deel werd verlaten. De laatste besmetting werd op 25 november 1976 geregistreerd.
Tijdens deze uitbraak werden 284 slachtoffers geregistreerd, waarvan 151 overleden. De oorzaak van de besmetting werd gezocht in het contact tussen mensen en ongedierte in de katoenfabriek zoals de zwarte rat, vleermuizen, de Tadarida trevori en steekmuggen.
Aanvankelijk werd aangenomen dat deze epidemie de waarschijnlijke bron was voor de uitbraak van de ziekte in Zaïre in hetzelfde jaar.[10] Argument hiervoor was de sterke mobiliteit van mensen tussen Nzara en de Bumba-regio in Zaïre. Jaren later bleek het echter te gaan om twee afzonderlijke soorten van het ebolavirus, waarbij het Sudan ebolavirus verantwoordelijk was voor deze epidemie.[11]
Zaïre[bewerken | brontekst bewerken]
In het noorden van het toenmalige Zaïre, het huidige Congo-Kinshasa, brak in de periode 1 september tot 24 oktober 1976 een epidemie van ebola uit. Hierbij werden 318 besmettingen, waarvan 280 doden, geregistreerd.
De epidemie begon in de Bumba-regio in de Evenaarsprovincie, nabij de stad Yambuku 95 km ten zuiden van de Ebolarivier. De eerste patiënt, een 44-jarige leraar op een missie-school, werd 1 september ziek nadat hij op 26 augustus een injectie met chloroquine tegen malaria had gekregen in een ziekenhuis van de Belgische missie in Yambuku. Ook anderen raakten ziek na deze injecties of na direct contact met andere besmette patiënten. Men ging er daarom van uit dat een gebrek aan hygiëne een rol speelde bij de verspreiding van de ziekte. Hierbij had de eerste patiënt de naald besmet, waarmee vervolgens ook anderen in het kader van vaccinatie werden geïnjecteerd.[12] Eind september werd ook een Belgische zuster ziek. Ze werd overgebracht naar het ziekenhuis in Kinshasa. Het ziekenhuis in Yambuku werd gesloten toen de epidemie zich verder uitbreide.
Op 3 oktober werd de Bumba-regio door de minister van Gezondheid in quarantaine geplaatst. Eind oktober was de epidemie uitgebreid tot acht dorpen.
Op het moment van de epidemie was de bron van de ziekte met verschijnselen van hemorragische koorts, hoofdpijn, buikpijn, misselijkheid, braken en bloedingen, onbekend. Wel werd in oktober bekend dat het virus verwant was aan het Marburgvirus. Belgische en Amerikaanse wetenschappers die werkzaam waren in het gebied ontdekten dat er sprake was van een nieuw virus. Ze noemden het virus naar de nabijgelegen Ebolarivier.[13]
Aanvankelijk dacht men dat de epidemie in Zaïre veroorzaakt werd door het ebolavirus wat verantwoordelijk was voor de epidemie in Soedan. Een aantal jaren later bleek echter het Zaïre ebolavirus, een soort van het ebolavirus, verantwoordelijk voor deze epidemie.[11]
2007[bewerken | brontekst bewerken]
In augustus 2007 heeft de Wereldgezondheidsorganisatie WHO een uitbraak van ebola geconstateerd in de Congolese provincie West-Kasaï. Er zouden minstens 167 mensen zijn bezweken na besmetting met het ebolavirus.
Op 29 november 2007 werd bekend dat in het district Bundibugyo in Oeganda op 10 november een ebola-uitbraak heeft plaatsgevonden.[14] Bij deze uitbraak ging het om een zelfs in 2010 nog onbekende variant van het virus.[15] Deze nieuwe variant heeft als kenmerk dat hij minder (externe) bloedingen veroorzaakt. Daarentegen lijkt het vooral een dodelijke variant te zijn door de koorts die het virus veroorzaakt. Door deze nieuwe variant zijn 66 mensen om het leven gekomen (mei 2019).[16]
2014[bewerken | brontekst bewerken]
West-Afrika[bewerken | brontekst bewerken]
De uitbraak van 2014 startte naar alle waarschijnlijkheid bij een jongetje van twee en zijn moeder uit de Guineese regio Guéckédou op 2 december 2013.[17][18] In maart 2014 stierven zeker 111 mensen in Guinee aan het virus en zijn er 127 geregistreerde geïnfecteerden.[19] Ook in buurland Liberia werden eind maart 2014 twee besmettingen met het virus vastgesteld.[20] Op 10 april 2014 werd vastgesteld dat er twee personen besmet zijn met ebola in Marokko, wat erop wees dat het virus zich verder verspreidde.[21] In juni 2014 telde men al 759 besmettingen waarvan 468 met een dodelijke afloop. Op 22 september 2014 waren er volgens de WHO al 5843 besmettingen bekend, waarvan 2803 patiënten zijn overleden. In Spanje is een besmette missionaris overleden aan de ziekte. Op 2 oktober 2014 liet de Wereldgezondheidsorganisatie weten dat het dodental reeds was opgelopen tot 3338 en het besmettingsaantal reeds 7178 bedroeg. In totaal zijn er 11.301 mensen overleden aan ebola, onder meer in Guinee (2536), Sierra Leone (3956) en Liberia (4809) en nog 15 mensen in andere landen (CDC, 17 feb 2016). Het aantal besmettingen ligt waarschijnlijk vele malen hoger, omdat niet alle gevallen vanwege de omvang van de epidemie kunnen worden geregistreerd.[22]
Congo[bewerken | brontekst bewerken]
In augustus werd ebola vastgesteld bij een zwangere vrouw die na het bereiden van bushmeat ziek was geworden. Ze overleed op 11 augustus. Door begrafenisrituelen zag het virus kans zich te verspreiden. Onderzoek toonde aan dat deze epidemie geen verband houdt met de uitbraak van ebola in West-Afrika.[23] In totaal vielen 49 doden.
2018-2020[bewerken | brontekst bewerken]
In 2018 heeft opnieuw een ebola-uitbraak in het oosten van Congo plaatsgevonden. De ziekte heerste vooral in het grensgebied met Uganda en Rwanda. Het aantal doden lag op 24 september van dat jaar op circa 100.[24] Op 17 juli 2019 lag het dodental op zeker 1.582 mensen en riep de WHO de uitbraak uit tot een medische noodsituatie ‘van internationale zorg’. Aanleiding was een ebola-overlijden in de miljoenenstad Goma, een grensplaats met Rwanda, op 200 km van de oorspronkelijke besmettingshaard. Op dat moment waren er al drie grensoverschrijdende sterfgevallen in Oeganda geweest.[22]
Op 13 december 2019 lag het dodental op 2.207.[25] Op 20 januari 2020 was dat licht gestegen tot 2.236.[26]
Vaccinatie en medicatie[bewerken | brontekst bewerken]
Antivirale middelen voor mensen die besmet zijn met ebola zijn in ontwikkeling. Nadat het virus in de Verenigde Staten in 1989 bij apen was geconstateerd is men hiernaar op zoek geweest. Na jaren van laboratoriumonderzoek is een vaccin gevonden dat bij muizen en waarschijnlijk ook bij apen werkt. Dit is echter nog niet volgens vastgelegde procedures op mensen getest. Zowel het Leidse bedrijf Crucell als het Canadese Tekmira Pharmaceuticals is ver met de ontwikkeling van een vaccin. Op 12 augustus schonk de Canadese regering aan de WHO ruim 1000 doses van haar experimentele ebolavaccin VSV-EBOV. Het vaccin was alleen nog getest op apen. De firma Janssen stelde op 28 oktober 2014 dat ze vanaf mei 2015 een miljoen vaccins zal produceren.[27] GlaxoSmithKline heeft inmiddels een vaccin dat met succes op 20 vrijwilligers is uitgetest, op basis van het verkoudheidsvirus van een chimpansee waaraan een niet-besmettelijk eiwit van het ebolavirus is toegevoegd.[28] Op 23 januari 2015 werd bekend dat de proefneming wordt voortgezet op grotere schaal in de getroffen gebieden in West-Afrika.[29] Uiteindelijk werd het vaccin van Merck getest bij 4000 mogelijk besmette vrijwilligers en bleek 100% effectief, mits op tijd toegediend.[30]
Begin augustus 2014 werd bekend dat twee Amerikanen, dr. Kent Brantly en Nancy Writebol, met succes[31] behandeld waren met het experimentele intraveneuze medicijn, een mengsel van drie monoklonale antilichamen, die na besmetting van muizen via de tabaksplant Nicotiana benthamiana kunnen worden verkregen,[32] genaamd ZMapp.[33][34] Ook de Spaanse priester Miguel Pajares is inmiddels behandeld met het experimentele middel.[35] Het middel was nog in de testfase bij dieren, maar is vanwege de ernst van de ziekte toch toegepast op drie doodzieke mensen en lijkt meteen veelbelovend te zijn.[36] Op 12 augustus overleed de Spaanse priester Miguel Pajares alsnog. Hij was al ernstig verzwakt voordat het medicijn werd toegediend.[37] Op 12 augustus maakte het bedrijf Mapp Bio bekend de kleine voorraad aan ZMapp gratis naar Liberia te sturen.[38] Drie lokale dokters leken daar met succes te zijn behandeld,[39] maar één van hen is toch overleden.[40]
Het middel TKM-Ebola, dat de FDA eerder in 2014 verbood toe te passen bij gezonde vrijwilligers, werd op 7 augustus vrijgegeven voor gebruik bij besmette personen.[41] Het geneesmiddel hindert de RNA-synthese van het virus en belet zo de aanmaak van ziekmakende eiwitten.[42]
Van de reeds bestaande geregistreerde geneesmiddelen bleek clomifeen veelbelovend in besmette muizen,[43][44] evenals het verwante toremifene.[45] Ook het niet-geregistreerde favipiravir was werkzaam tegen het virus in studies in vitro en met besmette muizen.[46][47] Het wordt uitgeprobeerd in Guinee.[48] Het bleek in februari 2015 matig effectief, vooral bij niet al te zwaar geïnfecteerde patiënten.[49]
Ook brincidofovir, een prodrug, ontwikkeld tegen andere virussen en in fase-3-onderzoek, werd in 2014 en 2015 uitgeprobeerd, maar de verantwoordelijke farmaceut zette deze experimentele fase stil vanwege te weinig proefpersonen met ebola.[50][51] In Liberia is met relatief succes lamivudine gebruikt. Dat middel is al geregistreerd bij hiv-infecties.[52][53]
Er zijn geen gevallen bekend van personen die na het genezen van dit virus een tweede keer ziek zijn geworden. Gelet op het geringe aantal besmettingen per uitbraak is dat ook niet verwonderlijk. Het is hierdoor echter niet duidelijk of het menselijk immuunsysteem op termijn zichzelf afdoende tegen het virus kan beschermen, zoals bij een gewone griep wel het geval is. Wel zijn gevallen beschreven van besmette personen die herstelden na bloedtransfusies met bloed van lotgenoten die eerder de ziekte hadden overleefd.[54] In Liberia komt in november 2014 volgens de WHO een dergelijk serum klaar voor gebruik.[55] In Guinee doet het Instituut voor Tropische Geneeskunde in Antwerpen een onderzoek met antilichamen uit bloed van genezen patiënten.[56]
In augustus 2019 werd bekend dat Ridgeback Biotherapeutics, een bedrijf uit Florida, een werkend medicijn zou hebben tegen ebola.[57]
Externe link[bewerken | brontekst bewerken]
- Ebola bij het Rijksinstituut voor Volksgezondheid en Milieu
- over de ontdekking van ebola van Andere Tijden
- Factsheet over ebola van de Wereldgezondheidsorganisatie
| [weergeven]Bibliografische informatie |
|---|
Chronische myeloïde leukemie
| Neem het voorbehoud bij medische informatie in acht. Raadpleeg bij gezondheidsklachten een arts. |
Chronische myeloïde leukemie | ||||
 | ||||
een afbeelding gemaakt met FISH | ||||
| Coderingen | ||||
| ICD-10 | C92.1 | |||
| ICD-9 | 205.1 | |||
| ICD-O | 9875/3 | |||
| MeSH | D010677 | |||
| ||||
Chronische myeloïde leukemie,[1] ook wel CML,[1] is een vorm van leukemie waarbij er een overmatige productie is van witte bloedcellen. Bij 95% van CML-patiënten wordt ook het Philadelphia chromosoom gevonden, een genetische abnormaliteit die kan ontstaan door straling (onder andere als gevolg van bestraling van andere kankervormen).
CML is een zeldzame ziekte. Per jaar komen er in Nederland zo’n 200-250 patiënten bij. De meeste patiënten zijn te vinden in de leeftijdsgroep van 50 tot 60 jaar. CML komt vaker voor bij mannen dan bij vrouwen.
Als medicijn kan imatinib worden toegediend waarvoor een studie in het New England Journal of Medicine een vijfjaarsoverleving van 89% laat zien.[2] Ook de weesgeneesmiddelen Dasatinib (Sprycel) en Nilotinib (tasigna) kunnen gebruikt worden als remmende medicatie van deze afwijking.
Externe link[bewerken | brontekst bewerken]
Literatuurverwijzingen[bewerken | brontekst bewerken]
- ↑ a b Everdingen, J.J.E. van, Eerenbeemt, A.M.M. van den (2012). Pinkhof Geneeskundig woordenboek (12de druk). Houten: Bohn Stafleu Van Loghum.
- ↑ Druker BJ, Guilhot F, O'Brien SG et al (2006) . Five-Year Follow-up of Patients Receiving Imatinib for Chronic Myeloid Leukemia. New England Journal of Medicine 355 (20): 2408–2417 . PMID: 17151364. DOI: 10.1056/NEJMoa062867.
Chronische lymfatische leukemie
| Neem het voorbehoud bij medische informatie in acht. Raadpleeg bij gezondheidsklachten een arts. |
Chronische lymfatische leukemie | ||||
 | ||||
Bloedmonster met CLL-cellen | ||||
| Coderingen | ||||
| ICD-10 | C91.1 | |||
| ICD-9 | 204.1 | |||
| ICD-O | 9823/3 | |||
| ||||
Chronische lymfatische leukemie[1] of CLL[1] is een type bloedkanker (in medische terminologie leukemie genoemd) waarbij te veel witte bloedcellen (lymfocyten) worden aangemaakt. Hoewel de maligne lymfocyten bij CLL er gewoon uitzien onder een microscoop, zijn ze dat niet en kunnen de lymfocyten infecties niet effectief bestrijden. CLL wordt tot maligne lymfomen gerekend en is de meest voorkomende vorm van leukemie bij volwassenen, waarbij mannen twee keer zo vaak CLL ontwikkelen als vrouwen. Meer dan driekwart van de nieuwe gevallen wordt gediagnosticeerd bij patiënten boven de 50 jaar. Hoewel CLL over het algemeen als niet te genezen wordt beschouwd, schrijdt de ziekte doorgaans langzaam voort, soms zelfs gedurende tientallen jaren.
Externe links[bewerken | brontekst bewerken]
- CLL Topics
- CLL Research Consortium
- Leukemia & Lymphoma Society
- Lymphomation.org
- US National Cancer Institute
- CLLResearch
- Stichting Contactgroep Leukemie
Zie ook[bewerken | brontekst bewerken]
| Bronnen, noten en/of referenties |
Acute lymfatische leukemie
| Neem het voorbehoud bij medische informatie in acht. Raadpleeg bij gezondheidsklachten een arts. |
Acute lymfatische leukemie | ||||
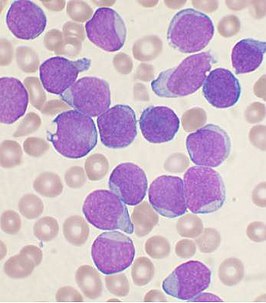 | ||||
| Coderingen | ||||
| ICD-10 | C91.0 | |||
| ICD-9 | 204.0 | |||
| ICD-O | M9835/3 | |||
| DiseasesDB | 195 | |||
| eMedicine | med/3146ped/2587 | |||
| MeSH | D054198 | |||
| ||||
Acute lymfatische leukemie, ook acute lymfoblastische leukemie of acute lymfoïde leukemie (ALL), is een acute vorm van leukemie (kanker van de witte bloedcellen) die gekenmerkt wordt door een overproductie en stapeling van maligne onvolgroeide witte bloedcellen ofwel lymfoblasten. Bij patiënten met ALL worden in het beenmerg continu lymfoblasten geproduceerd, waarbij de productie van normale cellen (bloedplaatjes, rode en witte bloedlichaampjes) verhinderd wordt en de ziekte zich verspreidt naar andere organen. ALL komt het meest voor bij kleine kinderen tussen 2 en 5 jaar en eveneens op hoge leeftijd.
Zie ook[bewerken | brontekst bewerken]
Acute myeloïde leukemie
| Neem het voorbehoud bij medische informatie in acht. Raadpleeg bij gezondheidsklachten een arts. |
Acute myeloïde leukemie | ||||
 | ||||
Beenmerg met acute myeloïde leukemie. Pijlen geven de Auer rods aan. | ||||
| Coderingen | ||||
| ICD-10 | C92.0 | |||
| ICD-9 | 205.0 | |||
| ICD-O | M9861/3 | |||
| OMIM | 602439 | |||
| DiseasesDB | 203 | |||
| eMedicine | med/34 | |||
| MeSH | D015470 | |||
| ||||
Acute myeloïde leukemie[1] (AML[1]) of acute myeloblastenleukemie[1] is een vorm van kanker die speficiek de myeloïde lijn van de witte bloedcellen aantast. Deze myeloïde lijn staat in voor de vorming van granulocyten, monocyten, erytrocyten en megakaryocyten. AML leidt tot een enorme proliferatie van onrijpe voorstadia van deze cellen in het beenmerg en meestal ook in het bloed (leukocytose). Het snel doordringen van abnormale cellen in het beenmerg interfereert met de normale vorming van bloedcellen (hematopoëse). De symptomen van AML worden veroorzaakt door het vervangen van normale beenmergcellen met leukemische cellen. Dit leidt ertoe dat de normale productie van rode bloedcellen (erytrocyten), bloedplaatjes en normale witte bloedcellen (leukocyten) in het gedrang komt. De symptomen omvatten moeheid, kortademigheid, blauwe plekken, bloedingsneiging en een toegenomen risico op infectie.
AML is de meest voorkomende vorm van acute leukemie bij volwassenen, met een incidentie die toeneemt met de leeftijd. Hoewel AML een betrekkelijk weinig voorkomende aandoening is is het verantwoordelijk voor ca. 1,2% van de sterfte aan kanker in de VS.[2] Door de toenemende vergrijzing van de bevolking wordt verwacht dat de incidentie van deze aandoening zal stijgen.
Hoewel verscheidene risicofactoren voor AML zijn reeds geïdentificeerd, blijft de oorzaak van de ziekte tot op heden grotendeels onbekend. Omdat het een acute leukemie betreft is de ziekte snel progressief. Typisch overlijdt de patiënt binnen enkele weken tot maanden indien de ziekte onbehandeld blijft. De vijfjaarsoverleving bedraagt 15 à 70%, afhankelijk van het subtype AML. AML wordt initieel behandeld met chemotherapie met als doel de ziekte in remissie te brengen. Vervolgens ontvangen patiënten additionele chemotherapie of een hematopoëtische stamceltransplantatie. Recente onderzoeken naar de genetica achter AML leidde tot de beschikbaarheid van tests die de werkzaamheid van bepaalde medicijnen voor een individuele patiënt kunnen beoordelen.
Epidemiologie[bewerken | brontekst bewerken]
Acute myeloïde leukemie is een zeldzame aandoening met ongeveer 3.7/100 000 nieuwe gevallen per jaar.[3] De aandoening komt voornamelijk voor bij ouderen, de mediane leeftijd bij het stellen van de diagnose ligt op 63 jaar. AML maakt 80% uit van de acute leukemieën bij volwassenen.[4] Mannen zijn iets meer aangedaan dan vrouwen (verhouding 1,3/1).[5] Op de kinderleeftijd hebben slechts 15 à 20% van de patiënten met acute leukemie AML. In het zeldzame geval dat AML bij een boreling aanwezig is, betreft het echter vrijwel steeds AML.
Het aandeel van AML ten gevolge van een voorgaande behandeling met chemotherapie is stijgende; op dit moment zijn 10 à 20% van de gevallen van AML het gevolg van deze behandeling.[6]
Er is enige geografische variatie merkbaar in de incidentie van AML. Bij volwassenen wordt de hoogste prevalentie gezien in Noord-Amerika, Europa en Oceanië. AML is zeldzamer in Azië en Latijns-Amerika.[7][8] In tegenstelling hiermee komt AML op kinderleeftijd minder voor in Noord-Amerika en India dan in andere delen van Azië.[9] Deze verschillen zijn mogelijk het gevolg van genetische factoren op populatieniveau, omgevingsfactoren of een combinatie van beide.
AML is in verband gebracht met genetische afwijkingen zoals (trisomie 21 (het syndroom van Down), Fanconi-anemie en het syndroom van Bloom. Verder worden omgevingsfactoren genoemd zoals de blootstelling aan bepaalde chemische stoffen, stralen, tabak en chemotherapeutica. Hematologische aandoeningen die in verband gebracht worden met AML zijn paroxismale nocturnale hemoglobinurie en de kwaadaardige aandoeningen myelodysplastisch syndroom en andere myeloproliferatieve aandoeningen.[10]
Klinisch beeld[bewerken | brontekst bewerken]
De meeste symptomen bij AML worden veroorzaakt door de vervanging van normale bloedcellen (rode bloedcellen, witte bloedcellen en bloedplaatjes) door leukemische cellen. Klachten die hiermee gepaard gaan zijn zwakte en vermoeibaarheid, infecties en het oplopen van blauwe plekken, tandvleesbloedingen, ecchymose, epistaxis of menorragie. Vaak komen deze klachten in combinatie voor.[10]
Koorts[bewerken | brontekst bewerken]
Eventueel aanwezige koorts kan in de meeste gevallen in verband worden gebracht met een infectie. Het beleid is afhankelijk van het al dan niet aanwezig zijn van neutropenie (< 1000 neutrofielen/μl), waarbij prompte toediening van een breedsprectumantibioticum geïndiceerd is. Indien geen duidelijke neutropenie aanwezig is bestaat nog steeds de mogelijkheid van functionele neutropenie. Hierbij zijn er normale hoeveelheden neutrofielen, doch zijn deze niet functioneel. Wanneer een bloeduitstrijkje microscopisch beoordeeld wordt en de neutrofielen hierbij bepaalde kenmerken tonen (zoals een hypogranulair aspect tonen of dysplasie), is dit suggestief voor functionele neutropenie. Op basis van een dergelijke functionele neutropenie kan eveneens overwogen worden antibiotica toe te dienen.[10]
Leukemie kan op zich ook aanleiding geven tot koorts, zelfs in de afwezigheid van een infectie. Dit is eerder het geval bij acute promyelocytaire leukemie.[11]
Huid[bewerken | brontekst bewerken]
Het verlaagd aantal bloedcellen kan tot bepaalde manifestaties leiden in de huid. Anemie, ten gevolge van een verlaagd aantal rode bloedcellen, leidt tot een bleke huid. Een verlaagd aantal bloedplaatjes leidt tot petechieën en ecchymosen. AML tast in 13% van de gevallen de huid zelf aan. Dit heet leukaemia cutis. Hierbij kunnen enkele of meerdere rode tot paarsblauwe papels, plaques of noduli ontstaan. Een andere verschijningsvorm is een roodbruine maculopapulaire eruptie. Het tijdsverloop tussen de diagnose en het verschijnen van de eerste manifestaties van de ziekte op de huid varieert sterk. Soms is leukaemia cutis het eerste symptoom van de ziekte.[12]
Gewrichten[bewerken | brontekst bewerken]
Ongeveer 4%-13%[10][13][14] van de patiënten met AML presenteren zich met gewrichts- en of botpijn. Dit ongemak doet zich voor in meerdere gewrichten, is doorgaans symmetrisch en kan migreren naar andere gewrichten.
Indien er pijnlijke, gezwollen gewrichten aanwezig zijn in het kader van een in het beenmerg en/of bloed aangetoonde leukemie, spreekt men over leukemische artritis. Andere oorzaken die tot deze artritis zouden kunnen leiden dienen dan echter uitgesloten te zijn. Een dergelijke leukemische artritis komt vaker voor bij kinderen met leukemie dan bij oudere patiënten[14] en vaker in het kader van een acute leukemie. Leukemische artritis kan zich reeds voor de diagnose leukemie werd gesteld presenteren, of later in het beloop van de ziekte de kop opsteken.
Expansie van het beenmerg kan eveneens aanleiding geven tot botpijn, deze oorzaak dient men echter steeds te onderscheiden van leukemische artritis, hoewel beide oorzaken wel samen kunnen voorkomen.
Externe link[bewerken | brontekst bewerken]
Literatuurverwijzingen[bewerken | brontekst bewerken]
- ↑ a b c Everdingen, J.J.E. van, Eerenbeemt, A.M.M. van den (2012). Pinkhof Geneeskundig woordenboek (12de druk). Houten: Bohn Stafleu Van Loghum.
- ↑ Jemal A, Thomas A, Murray T, Thun M (2002) . Cancer statistics, 2002. CA Cancer J Clin 52 (1): 23–47 . PMID: 11814064. DOI: 10.3322/canjclin.52.1.23.
- ↑ Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J., Harrison's principles of internal medicine, 17th. McGraw-Hill Medical Publishing Division, New York (2008), “chapter 104: Acute and Chronic Myeloid Leukemia”, p. 677-683. ISBN 9780071466332.
- ↑ Yamamoto JF, Goodman MT (2008) . Patterns of leukemia incidence in the United States by subtype and demographic characteristics, 1997-2002.. Cancer Causes Control 19 (4): 379-390 . PMID: 18064533.
- ↑ Greenlee RT, Hill-Harmon MB, Murray T, Thun M (2001) . Cancer statistics, 2001. CA Cancer J Clin 51 (1): 15–36 . PMID: 11577478. DOI: 10.3322/canjclin.51.1.15.
- ↑ Leone G, Mele L, Pulsoni A, Equitani F, Pagano L (1 October 1999) . The incidence of secondary leukemias. Haematologica 84 (10): 937–45 . PMID: 10509043.
- ↑ Linet MS, Monographs in Epidemiology and Biostatistics. Oxford University Press, New York (1985), “The leukemias: Epidemiologic aspects.”, p. I. ISBN 0195034481.
- ↑ Aoki K, Kurihars M, Hayakawa N, et al., Death Rates for Malignant Neoplasms for Selected Sites by Sex and Five-Year Age Group in 33 Countries 1953–57 to 1983–87. University of Nagoya Press, International Union Against Cancer, Nagoya, Japan (1992).
- ↑ Bhatia S, Neglia JP (1995) . Epidemiology of childhood acute myelogenous leukemia. J. Pediatr. Hematol. Oncol. 17 (2): 94–100 . PMID: 7749772. DOI: 10.1097/00043426-199505000-00002.
- ↑ a b c d Schiffer CA, Anastasi J, UpToDate. UpToDate, Waltham, MA, “Clinical manifestations, pathologic features, and diagnosis of acute myeloid leukemia”.
- ↑ Daly PA, Schiffer CA, Wiernik PH (1980) . Acute promyelocytic leukemia--clinical management of 15 patients.. Am J Hematol. 8 (4): 347-359 . PMID: 6932177.
- ↑ Kaddu S, Zenahlik P, Beham-Schmid C, Kerl H, Cerroni L (1999) . Specific cutaneous infiltrates in patients with myelogenous leukemia: A clinicopathologic study of 26 patients with assessment of diagnostic criteria.. Journal of the American Academy of Dermatology 40 (6): 966-978 . PMID: 20104987. DOI: 10.1016/S0190-9622(99)70086-1.
- ↑ Biswas S, Chakrabarti S, Chakraborty J, Paul PC, Konar A, Das S (2009) . Childhood acute leukemia in West Bengal, India with an emphasis on uncommon clinical features.. Asian Pac J Cancer Prev. 10 (5): 903-906 . DOI: 10.1016/S0190-9622(99)70086-1.
- ↑ a b Evans TI, Nercessian BM and Sanders KM (1994) . Leukemic arthritis. Semin Arthritis Rheum. 24 (1): 48-56 .
Coronaviridae
| Coronaviridae | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Taxonomische indeling | |||||||||||
| |||||||||||
| Soort | |||||||||||
| Coronaviridae | |||||||||||
| Afbeeldingen op | |||||||||||
| Coronaviridae op | |||||||||||
| |||||||||||
Coronaviridae vormt een familie van RNA-virussen met een omhulsel en positief enkelstrengs RNA. Het viraal genoom van deze virussen heeft een lengte van 26.000 tot 32.000 basenparen. Het virus is typisch bekleed met grote (~20 nm), knots- of bloemblad-vormige oppervlakte-projecties (de “peplomeren” of “spikes”), welke in elektronen-micrografie een afbeelding creëren die vergelijkenis vertoont met de corona van de zon of met een kroon (in Latijn corona). In het Nederlands worden de virussen van deze familie coronavirussen genoemd, maar deze naam verwijst vooral naar de leden van de onderfamilie Orthocoronavirinae.
Begin 2020 kreeg deze familie van virussen wereldwijd aandacht in verband met de pandemie van het COVID-19-virus, alsmede de theorie dat dit virus oorspronkelijk vleermuizen als gastheer moet hebben gehad.[1][2]
Taxonomie[bewerken | brontekst bewerken]
De familie Coronaviridae is georganiseerd in 2 onderfamilies, 5 genera (geslachten), 23 ondergenera en telt zo'n 40 soorten:
- Coronaviridae
- Letovirinae
- Orthocoronavirinae
- Alphacoronavirus
- Betacoronavirus
- Embecovirus
- Hibecovirus
- Merbecovirus
- Nobecovirus
- Sarbecovirus
- SARS-gerelateerd coronavirus (SARSr-CoV)
- SARS-coronavirus (SARS-CoV)
- SARS-coronavirus-2 (SARS-CoV-2)
- SARS-gerelateerd coronavirus WIV1 (SL-CoV-WIV1)
- SARS-gerelateerd coronavirus (SARSr-CoV)
Bronnen, noten en/of referenties
|
| Coronavirussen |
|---|
Ziekten bij mensen: COVID-19 · SARS · MERS |
Coronavirussen
| Coronavirussen | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | |||||||||||||
| Coronavirussen zijn virussen waarbij een corona (krans) te zien is wanneer ze door een elektronenmicroscoop worden bekeken. | |||||||||||||
| Taxonomische indeling | |||||||||||||
| |||||||||||||
| Onderfamilie | |||||||||||||
| Orthocoronavirinae | |||||||||||||
| Synoniemen | |||||||||||||
| |||||||||||||
| Afbeeldingen op | |||||||||||||
| |||||||||||||
De coronavirussen zijn een onderfamilie van virussen met positief enkelstrengig RNA als genetisch materiaal. Ze danken hun naam aan de krans (in het Latijn corona) rond de virusdeeltjes (virions). In de taxonomie vormen de echte coronavirussen de Orthocoronavirinae, tot en met 2018 de Coronavirinae genoemd. Dit is een onderfamilie van de Coronaviridae in de orde der Nidovirales.[2] Vroeger werd de naam coronavirussen ook wel gebruikt voor alle Coronaviridae.
De groep "voorheen ongekarakteriseerde menselijke ademhalingsvirussen" werd voor het eerst geïdentificeerd in 1966 door June Almeida, een Schotse virologe, terwijl ze samenwerkte met David Tyrrell (toenmalig directeur van het Common Cold Research Centre in Salisbury in Wiltshire).[3] Tyrrell stelde voor om de nieuwe groep "coronavirussen" te noemen.
[bewerken | brontekst bewerken]
Het belang van coronavirussen als ziekteverwekker bij de mens is moeilijk te evalueren, omdat ze moeilijk te kweken zijn in een laboratorium. Coronavirussen zijn, naast de rhinovirussen, de veroorzaker van een groot percentage van gevallen van gewone verkoudheid bij volwassenen, met name in de winter en vroeg in de lente. Van de ruim 30 in het laboratorium geïsoleerde stammen van het coronavirus bestaan zeven varianten die de mens kunnen infecteren:
- HCoV-229E
- HCoV-OC43
- SARS-CoV (zie onder)
- HCoV-NL63 (zie onder)
- HKU1-nCoV
- MERS-CoV (zie onder)
- SARS-CoV-2 (zie onder), veroorzaakte in 2020 de coronapandemie waarbij mensen de ziekte COVID-19 kregen
SARS, MERS en SARS-CoV-2 kunnen dodelijke longontstekingen veroorzaken.
[bewerken | brontekst bewerken]
HCoV-NL63 werd eind 2004 geïdentificeerd in Nederland. Onderzoekers in New Haven (Connecticut) troffen het virus later ook aan in monsters die zij hadden afgenomen bij verkouden kinderen. Zij noemden hun virusstam het New Haven-coronavirus (HCoV-NH), maar meldden ook dat deze sterk overeenkwam met HCoV-NL63 en dus op z’n minst tot dezelfde soort behoorde.
SARS (Severe Acute Respiratory Syndrome)[bewerken | brontekst bewerken]
Het SARS-coronavirus (afgekort SARS-CoV) veroorzaakte in 2003 een epidemie in Azië waarbij ongeveer 800 mensen stierven.
MERS (Middle East respiratory syndrome)[bewerken | brontekst bewerken]
MERS-CoV, voorheen bekend als nieuw coronavirus 2012 en HCoV-EMC,[4] komt bij kamelen voor en kan op de mens worden overgedragen. Bij een epidemie midden mei 2014 had MERS zich verspreid van Europa tot Nieuw-Zeeland, met twee gevallen in Nederland (bedevaartgangers die naar Mekka en Medina in Saoedi-Arabië waren gereisd).[5] In 2015 dook het virus ook op in Zuid-Korea.
SARS-CoV-2 (SARS-CoronaVirus 2)[bewerken | brontekst bewerken]
Eind 2019 vond in de Chinese miljoenenstad Wuhan een uitbraak plaats van een luchtweginfectie waarvan een tot dan toe onbekende variant van het coronavirus de verwekker bleek.[6] Het virus werd aanvankelijk informeel het Wuhan-coronavirus genoemd, kreeg de tijdelijke naam 2019-nCoV[7] en later SARS-CoV-2 vanwege genetische overeenkomsten met het SARS-virus. De ziekte kreeg de naam COVID-19 (CoronaVirus Disease 2019).
De eerste besmettingen worden in verband gebracht met een vismarkt in Wuhan, waar illegaal ook levende zoogdieren werden verhandeld. De markt werd daarop gesloten. Infectie met het virus veroorzaakt griepachtige symptomen en leidt bij sommige patiënten tot longontsteking, die dodelijk uit kan pakken. De Wereldgezondheidsorganisatie (WHO) beschouwde de uitbraak vanwege de snelle verspreiding en de ernst vanaf 30 januari 2020 als een wereldwijde medische noodsituatie.[8] Omdat er ook buiten China veel besmettingen plaatsvonden, merkte de Wereldgezondheidsorganisatie op 11 maart 2020 de epidemie aan als pandemie: de ‘coronapandemie’.
Zie ook[bewerken | brontekst bewerken]
- Lijst van virussen
- SARS-gerelateerd coronavirus WIV1
- Canine coronavirus
- Felien coronavirus
- Feliene infectueuze peritonitis
- Infectieuze bronchitis bij kippen
| Zie de categorie Coronaviridae van Wikimedia Commons voor mediabestanden over dit onderwerp. |
Noten
|
| Coronavirussen |
|---|
Ziekten bij mensen: COVID-19 · SARS · MERS |
Marburgvirus
| Marburgvirus | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
 | |||||||||||
| Marburgvirusdeeltjes, ~100,000x vergroot | |||||||||||
| Taxonomische indeling | |||||||||||
| |||||||||||
| Soort | |||||||||||
| Lake Victoria marburgvirus | |||||||||||
| Afbeeldingen op | |||||||||||
| Marburgvirus op | |||||||||||
| |||||||||||
Het marburgvirus is de veroorzaker van een ernstige en vaak dodelijke ziekte, die gepaard gaat met hevige bloedingen uit alle lichaamsopeningen.
Verspreiding[bewerken | brontekst bewerken]
Het zeldzame virus lijkt sterk op het ebolavirus: beide behoren tot de familie van filovirussen (Filoviridae), en de door het marburgvirus veroorzaakte ziekteverschijnselen lijken sterk op de ziekte die door het ebolavirus wordt veroorzaakt. Beide virussen zijn ook afkomstig uit dezelfde regio in Afrika: Oeganda en westelijk Kenia. De bron van het virus is een dierreservoir (zoönose). In 2006 werd bekend dat een buitenproportioneel groot aantal lijders was geassocieerd met grotten en mijnen, wat doet vermoeden dat de natuurlijke gastheer van het virus in een dergelijke omgeving moet leven.[1] Een team van onderzoekers uit de Verenigde Staten en Gabon ontdekte het virus inderdaad in de fruitetende vleermuizensoort Rousettus aegyptiacus (Nijlroezet).[2][3]
Structuur[bewerken | brontekst bewerken]
De structuur van het virus is karakteristiek voor filovirussen, met lange draadachtige virusdeeltjes die een constante diameter hebben maar die sterk in lengte variëren (800–1400 nm). De virusdeeltjes bevatten 7 bekende eiwitketens. Hoewel het marburgvirus sterk lijkt op het ebolavirus, treedt er geen kruisimmuniteit op: de twee virussen activeren twee verschillende antilichamen.
Geschiedenis[bewerken | brontekst bewerken]
Ontdekking[bewerken | brontekst bewerken]
Het marburgvirus was het eerste filovirus dat werd ontdekt. Het virus werd voor het eerst beschreven in 1967, toen 37 personen ziek werden in de Duitse steden Marburg en Frankfurt am Main, en in Belgrado (Joegoslavië). Het werd veroorzaakt door besmette Afrikaanse groene meerkatten (Cercopithecus aethiops) uit Oeganda, die werden gebruikt voor het ontwikkelen van vaccins tegen polio. De apen waren ingevoerd door Behringwerke, een Marburgse onderneming die was opgericht door de eerste Nobelprijswinnaar voor de Geneeskunde, Emil Adolf von Behring. De onderneming, die toentertijd onderdeel was van Hoechst, later van Dade Behring en daarna van Siemens, was oorspronkelijk opgericht voor het ontwikkelen van sera tegen tetanus en difterie.
Recente uitbraken[bewerken | brontekst bewerken]
Uitbraken van deze ziekte zijn bekend in 1967, 1975, 1980, 1987, 1998, 2004 en 2005. De meest recente uitbraak van het marburgvirus begon eind 2004 in het noorden van Angola en heeft tot en met 17 mei 2005 311 levens geëist bij 337 vastgestelde besmettingen. Buiten de provincie Uíge waren op dat moment al vijf weken geen nieuwe besmettingen vastgesteld. Een uitbraak in het naburige Democratische Republiek Congo tussen 1998 en 2000 eiste 123 levens. Een grotere uitbraak in Congo in 2000 eiste in drie weken tijd 140 slachtoffers.
Er zijn epidemiologen[bron?] die de hypothese hebben geopperd dat de zwarte dood die in de Middeleeuwen in Europa heerste en die sinds ca. 1900 altijd aan de pestbacil is toegeschreven wellicht helemaal niet door deze bacterie is veroorzaakt maar door een filovirus. Hiervoor zijn zeker ook argumenten te vinden. Dat het het marburgvirus zelf geweest zou kunnen zijn lijkt echter onwaarschijnlijk omdat de incubatietijd waarschijnlijk langer was.
In 2008 overleed een Nederlandse vrouw aan het virus. Zij heeft het waarschijnlijk opgelopen door contact met een vleermuis bij een bezoek aan een grot.[4] Mensen die met haar in contact zijn geweest zijn door het RIVM nauwlettend in de gaten gehouden. Er werd geen verdere besmetting geconstateerd.
Op 6 oktober 2014 werd een nieuw dodelijk slachtoffer van het marburgvirus gerapporteerd in Oeganda. Het slachtoffer was een 30-jarige radioloog die werkzaam was bij een ziekenhuis in Kampala. Hij overleed op 28 september aan de gevolgen van het virus. 80 andere personen werden uit voorzorg in quarantaine geplaatst.[5]
Symptomen[bewerken | brontekst bewerken]
De diagnose van het marburgvirus is moeilijk, omdat de ziekteverschijnselen aanvankelijk lijken op die van andere (besmettelijke) ziekten, zoals griep, malaria en tyfus.
De ziekte heeft een incubatietijd van 2 tot 10 dagen. Hierna volgen plotseling optredende koorts, hoofdpijn en spierpijn. Binnen een week ontwikkelt zich een maculopapulaire huiduitslag (huiduitslag met vlekken en knobbeltjes) gevolgd door braken, pijn in de borst, buikpijn en diarree. De ziekte kan vervolgens steeds ernstiger worden, en gepaard gaan met geelzucht, een delirium, gestoorde leverfunctie en omvangrijke bloedingen. Herstel van de ziekte duurt lang, er kunnen nog zwelling van de teelballen, terugkerende hepatitis, en ontstekingen van het ruggenmerg, de ogen of de speekselklieren optreden.
Mortaliteit[bewerken | brontekst bewerken]
De ziekte heeft een zeer hoge mortaliteit, die - afhankelijk van de beschikbare medische zorg - wordt geschat tussen de 25% en 92%.
Biologische oorlogsvoering[bewerken | brontekst bewerken]
In de jaren 80 experimenteerde de toenmalige Sovjet-Unie met het geschikt maken van het marburgvirus voor biologische oorlogsvoering. Dankzij Ken Alibek (voorheen Kanatjan Alibekov), een Sovjet-overloper die in 1992 naar de Verenigde Staten overliep, is meer bekend geworden over de Sovjet-activiteiten op dit gebied. Hij was de Eerste Onderdirecteur van Biopreparat, de organisatie die zich bezighield met het ontwikkelen van biologische wapens. Wetenschappers van Biopreparat ontdekten dat, in aerosolvorm, er slechts een paar virusdeeltjes nodig waren voor het infecteren van een slachtoffer. Ze onderzochten verder hoe dit virus met een intercontinentale raket van het type SS-18 ingezet kon worden tegen bevolkingscentra in NAVO-gebied. Nadat een van de wetenschappers, dr. Nikolai Ustinov, zichzelf per ongeluk geïnjecteerd had met Marburg, konden zijn collega's uit zijn stoffelijk overschot een nog dodelijkere versie van het virus isoleren en cultiveren. Deze werd variant U genoemd naar dr. Ustinov. Volgens Alibek waren de Sovjets in 1991 zover dat ze Marburg-variant U in grote hoeveelheden konden produceren. Volgens de plannen zouden dan tien afzonderlijk richtbare, met Marburg U geladen koppen op de genoemde raketten geplaatst worden die daarna in het operationele arsenaal van de Sovjets zouden worden opgenomen. Sinds het vertrek van Ken Alibek is weinig tot niets meer bekend over de status van het huidige Russische onderzoek naar en/of ontwikkeling van biologische wapens.[6]
Externe links[bewerken | brontekst bewerken]
- Info via WHO
- Informatie over filovirussen via RIVM
- Marburg fever in Uganda zoals vermeld bij NEWS24 oktober 2014
- CDC information on Marburg
- WHO: Marburg haemorrhagic fever in Angola - update
- Recombinomics: Marburg Virus Transmission in Angola Capital of Luanda 2005
Bronnen, noten en/of referenties
|



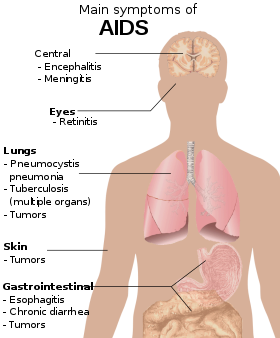




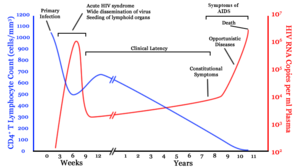



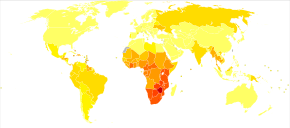





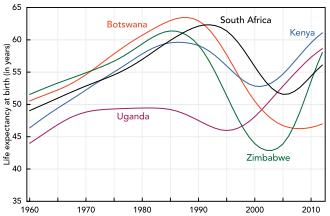

Comments
Post a Comment